Vascular depression for radiology: A review of the construct,methodology,and diagnosis
Sara N Rushia,Al Amira Safa Shehab,Jeffrey N Motter,Dakota A Egglefield,Sophie Schiff,Joel R Sneed,Ernst Garcon
Abstract
Key words: Vascular depression;Depression;Magnetic resonance imaging;Cerebrovascular disorders;White matter hyperintensities;Neuroradiology;Case reports
THE VASCULAR DEPRESSION CONSTRUCT
Vascular depression (VD) is a unique subtype of late-life depression (LLD). The VD construct consists of a group of patients with late-onset depression (LOD),structural brain changes characterized by higher rates of hyperintensities on T2-weighted brain magnetic resonance imaging (MRI),and greater neuropsychological impairment as compared to early-onset depression (EOD). Greater severity of MRI hyperintensities are associated with poor response to antidepressant treatmentand a more chronic course of depression. Therefore,the theory of VD suggests that LOD is a product of damage to corticostriatal circuits by cerebrovascular disease,which leads to executive dysfunction and poor antidepressant treatment response.
Cerebrovascular disease and depression
The VD subtype proposes that cerebrovascular disease is related to geriatric depressive syndromes,such that vascular risk factors lead to altered regional brain functioning,which leads to depression. However,there may be additional biological or genetic factors that are also determinants of VD. Indeed,there may be a strong genetic influence in the development of white matter hyperintensities (WMHs) in the elderly,and heritability of WMHs is estimated to be between 55% and 80%.Furthermore,there is an association between vascular risk factor burden and new onset of depression in the elderly population. LLD and cardiovascular disease share etiopathogenetic risk factors,such as high homocysteine levels and inflammation,which are also implicated in cognitive impairment. A meta-analysis found a significant association between vascular risk and LLD,with diabetes,heart disease,and stroke identified as strong individual correlates of LLD,and a recent study identified midlife cerebrovascular burden as a significant predictor of LLD,even after controlling for a history of depressive symptoms. A review of potential mechanisms underlying the VD construct proposed three hypotheses by which LLD is mediated:White matter disease leading to disrupted connections between brain areas associated with depression and cognition,inflammatory and immune processes leading to neurodegeneration,and reduced cerebral blood flow. However,the etiology of white matter hyperintensities in older depressed adults remains unclear. Depressed elders may have poorer blood flow to prefrontal tissue as cerebrovascular disease progresses. Additionally,the hippocampus is vulnerable to aging,and elders also experience reduced metabolism in limbic regions.
There is a consistent relationship between depression,vascular disease,and cerebrovascular risk factors. Indeed,cerebrovascular disease is commonly seen in MRI scans of depressed elders. In addition,considerable research has shown that ischemic cerebrovascular disease processes contribute to excessive deep WMHs(DWMHs). Thomasfound that all DWMHs in an elderly group with depression were ischemic,while less than a third of DWMHs in an elderly group with no depression were ischemic. However,Thomassuggested that the high frequency of ischemic lesions in depressed patients is not due to vascular disease,but instead due to a change in DWMHs from nonischemic to ischemic once a certain threshold for ischemic damage is surpassed. The mechanisms underlying the ischemic disease connected to DWMHs are nonspecific;potential pathways include poor endothelial functioning and increased atherosclerosis. Age-related changes in cerebral autoregulation and regulation of blood pressure may also lead to WMHs.These findings further promote the idea that subtle microvascular changes may be one reason why some people develop their first episode of depression later in life.
White matter disease is thought to damage white matter tracts and play a major role in the etiology of LOD by affecting the processes involved in emotional regulation. A meta-analysis of 30 studies found that individuals with LOD were over four times more likely to have significant white matter changes and greater lesion severity than those with EOD. These findings have also been replicated in a more recent meta-analysis. Vascular changes,particularly subcortical white and gray matter lesions,are associated with more severe depressive symptoms. Specifically,in elderly patients with late-onset as opposed to early-onset depressive disorders,deep white matter and basal ganglia hyperintensities are more prevalentand are associated with more severe symptoms and poorer prognosis. The corticostriato-pallido-thalamo-cortical pathways have been implicated as areas particularly affected by vascular disease in LLD. Additionally,Bellasuggest that patients exhibiting a VD profile have disruptions in the frontal subcortical circuits connecting the dorsolateral prefrontal cortex and dorsal section of the head of the caudate nucleus.
Vascular disease in treatment of depression
Vascular risk factors contribute not only to the pathogenesis of depression but also complicate its treatment. Several studies have suggested that older adults with greater WMH volume show a poorer response to antidepressants. In clinical samples,progression of white matter lesions has occurred alongside a lack of response to antidepressants and recurrence of depression. Patients with LLD with lacunar lesions,as opposed to diffuse white matter lesions,have shown a better response to antidepressant treatment,supporting the view that VD associated with white matter lesions is treatment-resistant. It is hypothesized that the pathology caused by the disruption of prefrontal systems related to white matter lesions is a central mechanism to why these patients do not respond to the typical antidepressant treatment. However,some studies have failed to find a connection between WMH severity and treatment outcomes.
Along with poorer response rates to antidepressants,white matter hyperintensity progression has been shown to predict poorer outcomes,higher rates of relapse,and difficulty achieving remission. Indeed,in a study of severely depressed psychiatric inpatients,those who responded to treatment showed significantly less white matter lesion burden. The presence of subcortical gray matter lesions predicted poor outcome up to 64 months following antidepressant monotherapy. Steffensfound that lesions in the basal ganglia and in the cerebral cortex were associated with the persistence of depressive symptoms,while subcortical white matter lesions were associated with worsening of depressive symptoms over time. Additionally,patients with VD are more likely to suffer from earlier relapse,have a more chronic pattern of depression,and have progressive cognitive decline.
Since current pharmacological treatments for depression have been primarily ineffective in VD patients,there is growing interest in controlling lesion progression.If white matter lesions can predict poor antidepressant response,targeting the cerebrovascular processes themselves might be more effective. Most studies of vascular depression are correlative and cannot determine causation. It is unknown if depression puts one at greater risk for developing white matter lesions,if the presence of microvascular ischemia makes one more susceptible to depression,or if both are the result of a common pathological pathway. Another possibility is that untreated depression itself quickens lesion progression and results in additional vascular disease,such as vascular dementia. In a retrospective cohort study of patients in primary care spanning 13 years,K?hlerfound that new onset of depression was associated with twice the likelihood of developing dementia,especially in those with incident vascular disease or whose depression was preceded by stroke or hypertension. Since the current standard psychopharmacologic therapy is ineffective and there are few placebo-controlled trials examining the effect of hyperintensities on antidepressant treatment response,there is a clear need for more careful clinical assessment and follow-up of those with lesion burden.
Vascular disease,vascular depression,and cognitive impairment
There is an established connection between vascular disease and the development of cognitive impairment (vascular dementia),which co-occurs with MDD at a rate of approximately 20%. Midlife vascular risk factors are also associated with elevated amyloid deposition in late-life. Furthermore,new onset of depression in adults with mild cognitive impairment was found to be associated with deep subcortical WMH severity. Puglisi and colleaguesfound that VD patients exhibit hemodynamic dysfunction,which may contribute to the development of cognitive impairment.Pennisi and colleaguesfound differences in intracortical facilitation between patients with VD and patients with vascular cognitive impairment at baseline but not at a two-year follow-up. While the vascular cognitive impairment group did not cognitively decline over the two years,the VD group did show evidence of cognitive decline. Thus,the researchers proposed that the hyperfacilitation observed in the vascular cognitive impairment group may have contributed to the preservation of cognitive functioning as compared to the VD group. They concluded that the risk of dementia in VD may be due to lack of compensatory functional cortical changes or subcortical vascular lesions. Thus,vascular depression might fall on a continuum that would include vascular disease,vascular depression itself,and vascular dementia. Indeed,case studies have reported progression from vascular depression to vascular dementia.
Vascular depression has been associated with cognitive impairment,most notably in executive functioning and psychomotor speed. Patients with MRI-defined VD were shown to have significantly more psychomotor retardation and significantly worse performance on the Stroop Color-Word Interference Testand the Initiation/Perseveration subtest of the Mattis Dementia Rating Scalethan non-VD patients. Poor performance on the interference component of the Stroop Color-Word Interference Test exemplifies that response inhibition is low for these patients. Since the inception of the concept of vascular depression,Krishnan and colleagues have redefined their idea into Subcortical Ischemic Depression (SID)and Alexopoulos and colleagues reconceptualized their model into the Depression-Executive Dysfunction Syndrome (DED). Both of these subtypes reflect different aspects of VD,and shed light on the neuropsychological deficits that arise when VD is defined by MRI or clinical presentation,respectively. Potterfound that patients with MRI-defined SID had an overall worse neuropsychological profile than depressed older adults without SID. Specifically,SID patients performed worse on measures of working memory and nonverbal memory,after controlling for age,cardiovascular risk,and depression symptoms. Alexopoulosfound that patients with DED had reduced fluency and visual naming,and psychomotor retardation. Interestingly,both SID and DED definitions predict functional disability at similar rates.
Similar patterns of cognitive impairment have been found for constructs that share symptomology with VD. Depressed elderly patients with white matter hyperintensities demonstrate deficits in processing speed and executive functioning.White matter abnormalities in depressed geriatric patients have also been associated with poor response inhibition as measured by the Stroop Color-Word Interference Test. Geriatric depressed antidepressant non-responders show deficits in verbal learning,psychomotor speed,and initiation and perseveration. Impairment in initiation and perseveration has also been associated with relapse and recurrence of LLD. Additionally,a meta-analysis of patients with LLD found that the executive functioning domains of planning and organization were associated with poor antidepressant treatment response. Vascular burden in adults with LLD was predictive of poor processing speed functioning after controlling for age,education,and depressive severity.
Additional clinical and physiological characteristics of VD
Patients with VD also display characteristics nonspecific to neuropsychological assessment. Older adults with VD have a lower rate of family history of mood disorders than older adults with depression and no vascular disease. Patients with vascular dysfunction and depression have demonstrated higher levels of aggressive and auto-aggressive tendencies and increased alexithymia. Additionally,VD patients have been shown to have more disability with activities of daily living than depressed geriatric patients without vascular disease. Other features of VD include apathy,lack of insight,and difficulties at work. Older adult women with high cerebrovascular burden and probable depression have been shown to be at a higher risk for later frailtyand subsequent shortened lifespan.
Furthermore,VD patients exhibit distinct physiological profiles. This includes specific patterns of motor cortex excitability,higher concentrations of inflammatory markers,and higher levels of plasma homocysteine. Research into the etiopathology of VD indicates that a genetic variation at aquaporin 4 (AQP4) locus may play a role. Sleep status between VD,non-vascular depression,and normal subjects has also been shown to differ,such that VD patients had higher rates of sleeprelated breathing disorders,daytime sleepiness,and disorders of 24-hour sleep structure.
METHODOLOGY OF WMH ASSESSMENT
In clinical practice,radiologists are often tasked to evaluate the brain MRI of patients with dementia for structural damages. Although the MRI findings alone are nonspecific,there are certain patterns of cerebral atrophy that may lead to additional investigations (.,PET,fMRI) in addition to the clinical and biological presentations for a definitive diagnosis. We believe that a similar approach can be done in vascular depression if a methodologic assessment of the cerebral white matter signal intensity on FLAIR is performed by the advised radiologists at the request of their referral practitioners.
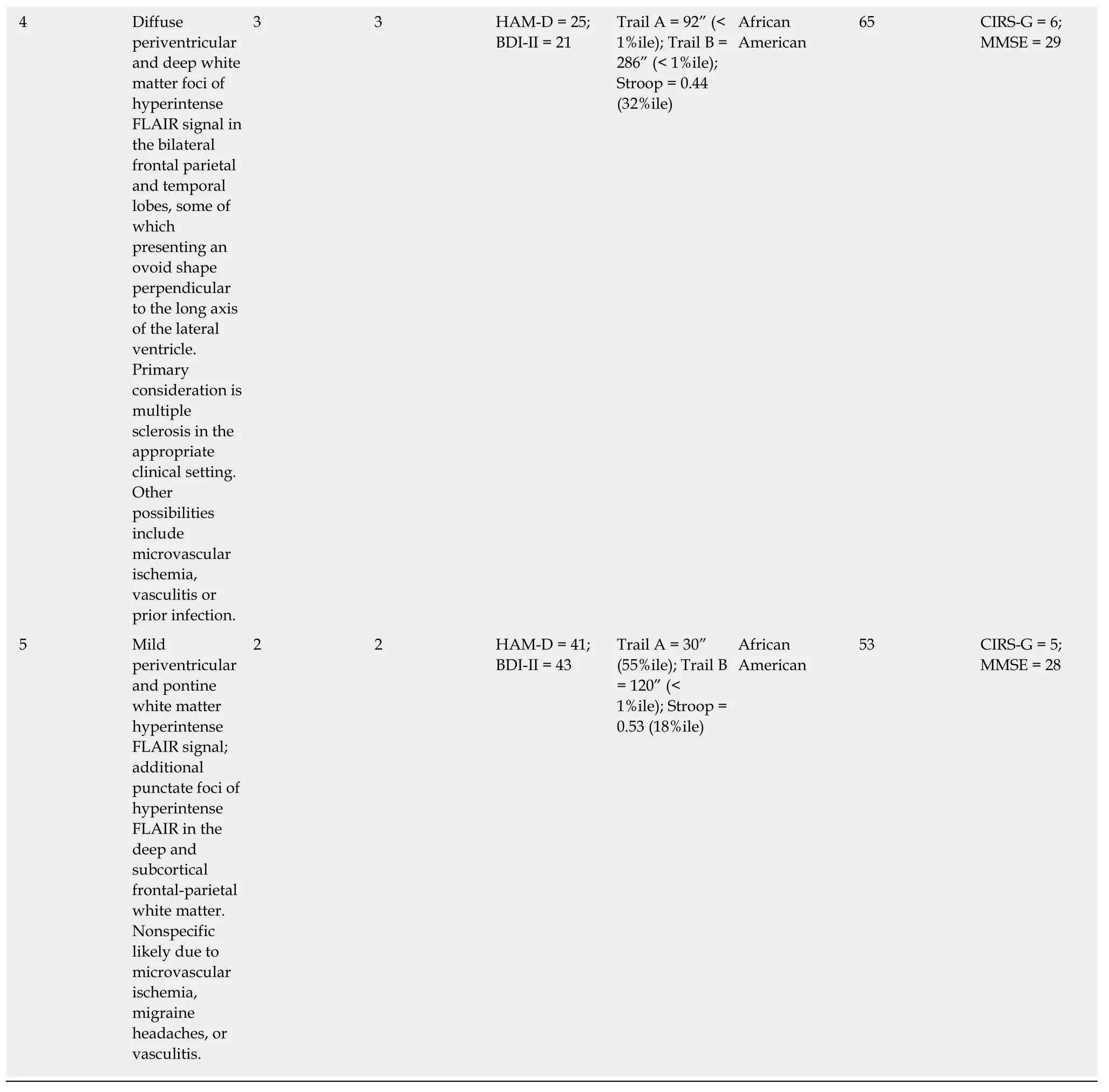
The quantification and localization of white matter hyperintensities is critical for research into the risk factors,etiology,and pathogenesis of VD. Thus,the validity of MRI-defined VD as a distinct diagnostic entity depends on the methodology that is used to characterize lesions. WMHs are typically analyzed using either semiquantitative ratings or quantitative volumetric analysis. Past research has primarily focused on WMH visual ratings or volume measurement without distinguishing among anatomically distinct WMHs,while recent studies have increasingly used semi-automated or fully automated methods to calculate WMH volume and classify WMHs into localized categories such as periventricular white matter hyperintensities(PVWMHs) and DWMHs (Figure 1). MRI hyperintensities most often have been scored for severity using visual rating scales including the Fazekas-modified Coffey rating scale,the Scheltens rating scale,the Boyko Pathology Rating Scale,and the Virchow-Robin spaces.
A fundamental issue in standardizing MRI-defined VD is how lesions in these patients are defined. For example,subcortical ischemic disease can involve white or deep gray matter,but VD research focuses primarily on white matter lesions.Hyperintensities can be divided according to location: Periventricular on the periphery of the lateral ventricles,deep white matter,or subcortical gray matter. It has been shown that deep white matter hyperintensities,though having a uniform appearance on conventional imaging,are histologically heterogeneous. WMHs may be considered periventricular if they are located within a certain distance from the lateral ventricles or remain contiguous as they spread away from the ventricles.Clear criteria for hyperintensities need to be operationalized so that research is conducted consistently.
The Fazekas-modified Coffey rating scale is commonly used in research evaluating VD. This scale measures hyperintensities in three locations on T2-weighted images: Deep white matter,subcortical gray matter,and periventricular spaces. Deep white matter hyperintensities in the frontal,parietal,temporal,or occipital lobes are scored as 0 (absent),1 (punctate foci),2 (beginning confluence of foci),and 3 (large confluent areas). Subcortical gray matter hyperintensities are abnormalities in the caudate nucleus,putamen,globus pallidus,thalamus,and internal capsule,and are scored as 0 (absent),1 (punctate),2 (multipunctate),and 3 (diffuse). Periventricular hyperintensities are abnormalities immediately adjacent to the lateral ventricles and are scored as 0 (absent),1 (caps),2 (smooth halo),and 3 (irregular and extending into the deep white matter). However,the Fazekas scale does not allow for detailed volumetric analysis of white matter hyperintensities.
The Scheltens rating scaleis based on the size and number of lesions in four separate regions: Periventricular white matter,deep white matter,basal ganglia,and infratentorial area. The periventricular white matter of the frontal caps and occipital caps and bands have ratings of 0 (none),1 (smooth halo,> 1-5 mm),and 2 (large confluent lesions,5-10 mm). The same rating system is used for the remaining three areas: The deep white matter of the frontal,parietal,occipital,and temporal lobes;the basal ganglia including the caudate nucleus,putamen,globus pallidus,thalamus,and internal/external capsule;and the infratentorial area consisting of the cerebellum,mesencephalon,pons,and medulla. The rating system ranges from 0 to 6 with the following descriptors: 0 (none),1 (≤ 4 mm and≤ 5),2 (≤ 4 mm and> 5),3 (4-10 mm and≤ 5),4 (4-10 mm and> 5),5 (≥ 10 mm and≥ 1),and 6 (confluent). However,this scale may underestimate the significance of punctate lesions since a score of 2 allows for infinite smaller lesions,whereas one large isolated lesion would be rated as a 5. Scheltens rating scales have a greater range than the Fazekas scale,yet Van Straatensuggest that the Fazekas scale is most appropriate for classifying different WMH groups.
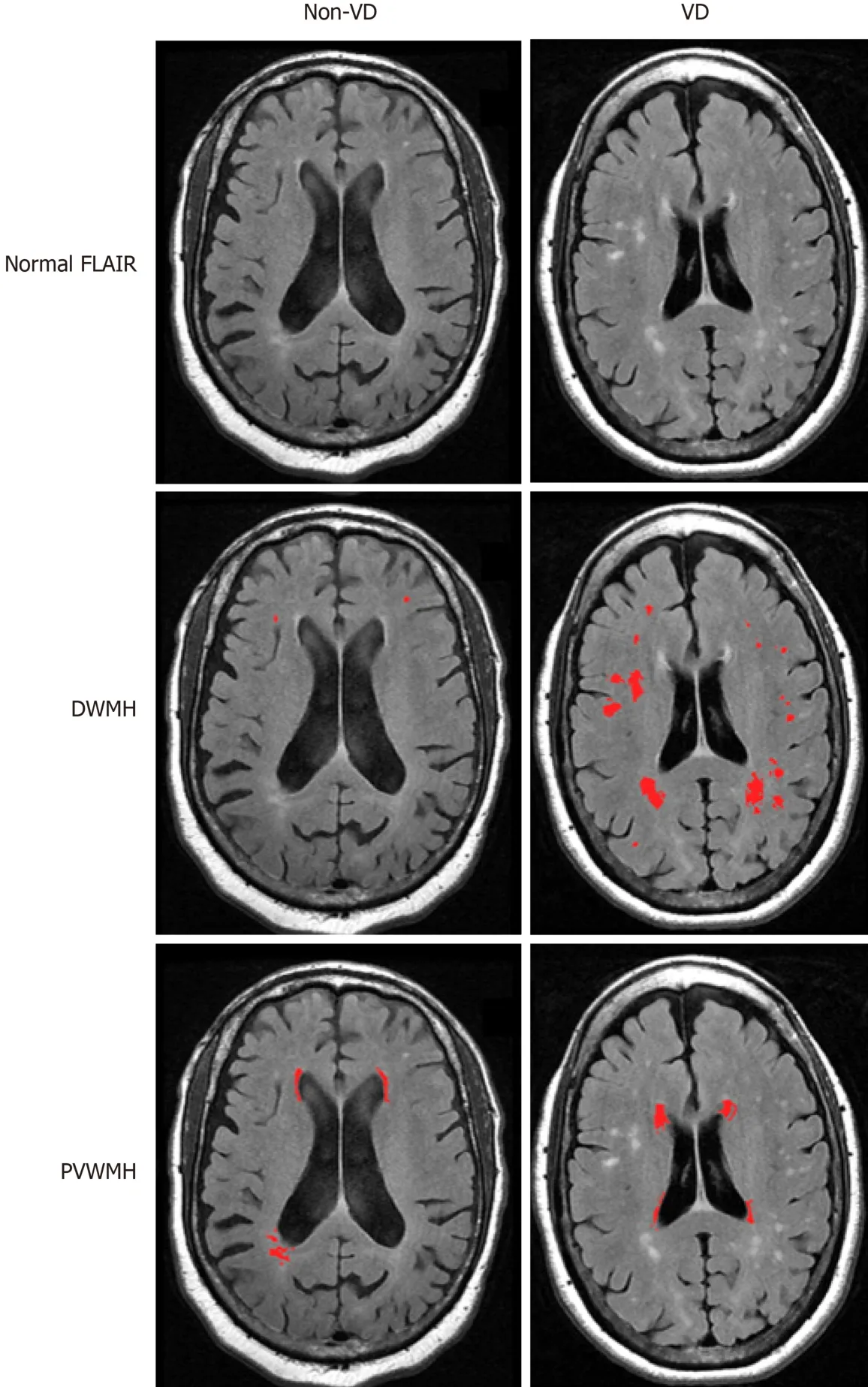
Figure1 Discrimination of vascular depression and non-vascular depression white matter hyperintensities.
Visual rating scales of WMHs are widely used because they are relatively easy to conduct and there are several scales available with demonstrated reliability and validity. In addition,visual rating scales allow expert raters to utilize clinical judgment to evaluate the specific lesion presentations and patterns. Van Straatenconfirmed correlations among WMH volume and the three most commonly used visual rating scales,but found greater variability and less correlation among scores in patients who had greater WMH burden.
Despite the advantages,visual scales are not well suited for measuring changes in lesions,and cannot quantify lesion volume. Visual scales can be time consuming,making them a poor choice for large datasets,and rely on clinical judgment,which can introduce issues concerning interrater reliability and validity. In addition,visual scales often do not include size and uniform location,making scores from different rating scales incomparable. Although visual scales allow differentiation between periventricular,deep white,and subcortical gray hyperintensity ratings,such classifications are inherently broad and imprecise. For example,WMHs adjacent to the left anterior horn of the lateral ventricle are combined with WMHs located in the right posterior horn of the lateral ventricle in the periventricular classification. Lesions in such disparate regions may have vastly different influences on cognition.
Recent imaging techniques have been developed to enable the quantitative volumetric analysis of signal hyperintensities that use semi-automated methods and provide more information on location and size,as well as continuous data. One method uses the software MRIcroto create a region of interest map by semiautomatic intensity thresholding(Figure 2). Separate region of interest (ROI)maps for different hyperintensity categories (deep white,periventricular,subcortical gray) are created by gross manual outlining of hyperintensities. The overlap of the intensity ROI and each hyperintensity category ROI is then used to compute the volume and location of the final lesion map. A principle advantage of semi-automated tracing is the ability to exclude areas that are typically hyperintense (.,pyramidal tracts and hippocampus) from total volume estimates. However,it is more time consuming than visual rating scales. For these reasons,it may be advantageously applied for medium,but not large datasets,where a fully-automated procedure may be more appropriate.
Fully-automated segmentation techniqueseliminate the interrater reliability problem because methods of lesion quantification are standardized and require little user intervention. Additional advantages include the production of quantitative data,the ability to analyze large data sets quickly,and the ability to recognize patterns.Quantitative ratings also allow for more precise measurement,and thus greater sensitivity to smaller lesions and different criteria for classification of white matter lesions. Since fully-automated segmentation techniques take place within MRI analysis software,the finalized lesion maps are amenable to realignment with standardized anatomical atlases. This facilitates ROI analyses that can be more spatially specific than analyses performed on qualitatively scored data. With these advantages,automated methods are potentially superior to visual rating scales for quantifying signal hyperintensities on MRI. Indeed,visual ratings may be less sensitive with the potential for ceiling effects and low discrimination of absolute lesion volumes. Disadvantages of automated methods include requiring computational sophistication,the correct software,and a level of user intervention and troubleshooting.
Fully-automated segmentation approaches also need to be evaluated for validity concerns. Validity may be in question because of the potential for interference effects by radiological artifacts. These artifacts may interfere with the segmentation process or with the steps needed to perform regional analyses. For example,fully-automated approaches rely on the brightness of adjacent pixels to identify lesion boundaries. This could lead to a problem in distinguishing pathological lesions from normal anatomical areas that are typically hyperintense (.,pyramidal tracts and hippocampus). Additionally,motion artifacts may invalidate fully automated analyses on scans that could otherwise be assessed manually on a qualitative rating scale. Therefore,the validity of MRI-defined VD relies on the reliability and validity of the rating scales and techniques used,which currently can still be inconsistent among research studies.
More recently,diffusion tensor imaging (DTI) has been used to examine the structural integrity of white matter areas relevant to LLD. In fact,it has been suggested that DTI may be more sensitive in identifying white matter damage than T2-weighted MRI. Fractional anisotropy has shown that white matter changes occur with aging,cognitive dysfunction,expressions of psychopathology,and LLD. Lower fractional anisotropy in the anterior thalamic radiation and superior longitudinal fasciculus,both projecting to the frontal lobe,has been associated with LOD,while lower fractional anisotropy in cortico-striato-limbic areas has been found in older adults who remained depressed after an antidepressant trial. DTI has revealed microstructural changes in the anterior cingulate cortex,superior and middle frontal gyrus,and right parahippocampal gyrus in association with LLD.Functional MRI (fMRI) has also been used to examine the relationship between white matter hyperintensities and LOD. Indeed,white matter lesions have been associated with altered functional connectivity in the brain in LLD. This research suggests that the use of DTI and fMRI techniques may be beneficial in examining vascular depression. Other newer imaging techniques such as MR perfusion have not yet been utilized in this population.
PATHOPHYSIOLOGY AND DIAGNOSIS OF VD
Vascular depression is often viewed solely from a geriatric psychiatry perspective.Typically,a clinical diagnosis is made after careful evaluations that include full physical and neuropsychological examinations,despite the possibility that a specific depression symptom profile might not constitute a clinical marker for VD. Vascular depression depends on the assessment of brain lesions and thus is ultimately a neuroradiological diagnosis.
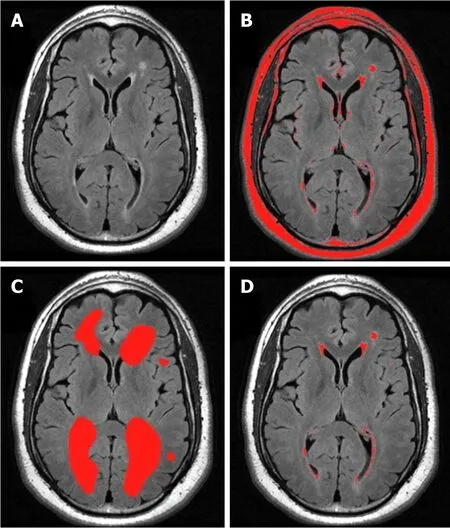
Figure2 Semi-quantitative method.
A number of researchers have proposed diagnostic criteria to define the VD subtype,but these have not always been consistent. Without consistent criteria,it is difficult to interpret conflicting findings,and since we do not know to what degree the possibly different patient groups overlap,there is no way to evaluate discrepant findings. To provide more clarity on this issue,Sneedevaluated patients with LLD and found that the vascular group was most accurately identified by DWMHs. Those in the vascular group were defined by a high probability of having MRI hyperintensities (DWM and periventricular),executive dysfunction,and late age-of-onset. These findings provide empirical evidence that VD is a unique subtype of LLD and the first empirically-based diagnostic criteria for VD.
WMH burden can be presented as volume,or as a proportion of the total white matter or intracranial volume,depending on the focus of the study. However,it remains unclear whether quantity or severity better accounts for predictive ability.Taylorfound that the overall percent increase in white matter hyperintensity volume had greater predictive significance of depressive symptoms and poor outcome than baseline volume. Others have reported similar results wherein greater changes in white matter presentation show greater symptoms and a more chronic course of illness. This suggests that total lesion volume at any particular time point is not nearly as important as the course of progression,and thus perhaps it may be more important to look at the specific areas in which the lesions are occurring.Quantity of lesions versus a certain pattern of lesions may also be related to clinical expression. Van Straatenquantified individual lesions to determine WMH severity,but the number of lesions was not related to depressive symptoms,suggesting that perhaps size of lesions is more relevant.
The significance of defined WMH locations has not been agreed upon,as it is unclear whether severity of overall lesion burden or lesion location is the dominant pathological contributor to vascular depression. Differences in WMH load between those with LOD and those with EOD have not consistently been found,suggesting that location of lesions,rather than quantity,might be more important in the differential diagnosis. Simpsonfound that hyperintensities were predictive of depressive symptomology when looking at specific areas such as the frontal lobes,basal ganglia,and pons,as opposed to total volume. On the other hand,a three-year follow-up study of a community cohort concluded that WMH severity was a strong predictor of depression risk,with half of MDD elderly meeting criteria for VD.Similarly,in a 12-wk antidepressant nonrandomized controlled trial,WMH severity was found to be associated with depression severity as well as vascular risk factors.Hickiereported no correlations between specific lesion locations and outcome,but rather that the burden of total white matter hyperintensity volume led to a poorer outcome in depressed patients. In addition,a two-year longitudinal study found that for every 1% increase in WMH volume,there was a 7% increased risk of poor prognosis.
The most consistently reported abnormality described in LLD is the increased number and/or severity of white matter hyperintensities,which mainly occur in subcortical gray and frontal white matter areas. It is thought that these changes represent vascular pathology in clinically relevant areas,though the debate about lesion severity and location remains. Rabinsshowed a particular dominance of lesions in the frontal lobes and basal ganglia. The locations of these lesions fit with functional imaging changes suggesting frontal and caudate abnormalities in depression,and further support the role of frontostriatal dysfunction in the vascular depression hypothesis. Many studies have focused on the significance of the frontal lobe in the physiopathology of LOD. MacFallfurther localized significant WMHs in depressed elders to the medial orbital prefrontal cortex. Other studies found that hyperintensities in the basal ganglia,particularly the putamen,predicted depressive symptoms and poorer treatment outcome. Lesions in the basal ganglia and subcortical gray matter were also shown to be predictive of failure to respond to treatment. Alexopouloslocalized WMHs to the frontal white matter lateral to the anterior cingulate cortex (ACC),which predicted lower remission rates after antidepressant treatment. More recently,increased low-theta activity in the subgenual ACC was found to be a possible predictor of antidepressant treatment response to repetitive transcranial magnetic stimulation in patients with treatmentresistant VD.
Vascular depression may affect different groups of older adults differently,and is likely overrepresented among African American older adults. In a sample of older adult depressed patients,61% of African Americans and 10% of Caucasians were classified as having VD. Additional evidence arises from research that shows that the rates of cardiovascular disease risk factors are significantly higher in African Americans compared to Whites. For instance,the rate of hypertension is significantly higher in African Americans (60%) than Whites (38%). African Americans are also more likely to have diabetesand significant health concerns for obesity.Indeed,cardiovascular disease is the leading cause of death in African Americans.People with diabetes,hypertension,or individuals that smoke are 2 to 4 times more likely to develop stroke than those without diabetes or hypertension,or nonsmokers. Additionally,stroke and stroke-related mortality rates are higher in African Americans compared to Whites across the lifespan. Stroke increases the risk for dementia,and in particular,vascular dementia. Indeed,the rate of vascular dementia is higher in African Americans relative to Whites. All of these cardiovascular risk factors combine to suggest that African Americans are at high risk for vascular depression.
Differential diagnosis for radiology
Neuroradiologists examining older adult scans do not typically consider vascular depression as part of the differential diagnosis. Mild and moderate white matter lesions are common in healthy elderly people and have unclear significance,but severe changes are not part of normal aging. White matter changes on MRI independently are of little clinical value to predict depressive symptoms. However,when viewed as a part of an entire clinical presentation,they raise suspicion for further depressive symptoms. For example,the rate of MRI hyperintensities has been found to be higher in populations with LLD compared to age-matched controls,while DWMHs are specifically prevalent in those with LOD. Thus,in practice it would be of clinical utility to take account of the presence of white matter changes on MRI when attempting to predict future depressive symptoms. This may influence decisions regarding the frequency of clinical monitoring and the need for prophylactic antidepressants or other treatments.
Neuropsychological assessments can also play a role in the diagnosis of VD.Impairments on tests that measure executive functioning,such as the Trail Making Testand the Stroop Color-Word Interference Test (Stroop Test),have been observed in individuals with diagnoses of VD. Trail A of the Trail Making Test assesses visual scanning,attention,and processing speed. Trail B of the Trail Making Test requires both sequencing and set shifting,and is used to assess divided attention and cognitive flexibility. Patients with lesions in the dorsolateral frontal areas have shown impairment as compared to control participants on the Trail Making Test,implicating executive dysfunction corresponding with the disruption of frontal areas.The Stroop Test is used to measure selective attention and response inhibition. Poor performance on the Stroop Test,especially on the interference condition,has been linked to frontal lobe dysfunction. However,it is possible that the Stroop Test activates a more distributed network of brain areas,including the middle frontal gyrus,parietal lobe regions,and temporal lobe regions. More distinguished evidence has been found specifically for anterior cingulate cortex activation during the interference condition.
The typical use of neuroimaging in psychiatry is to exclude structural lesions or other neurological pathology as causes for clinical presentation;neuroimaging has not yet played a major role in psychiatric diagnoses. Disagreement regarding which hyperintense signals should be viewed as pathological and how they should be graded may contribute to inconsistent diagnoses in this area. However,the evidence pointing to specific neuroimaging correlates of VD imply that a neuroradiological diagnosis or recommendation for a diagnosis can be made. Despite the possibility that radiologists might not have access to a patient's depressive symptomatology,neuropsychological performance,or history of illness,they can contribute to the diagnosis through their understanding of the nature of lesions in addition to the VD presentation. We offer some recommendations based on radiologists' comments on MRI scans that,associated with other data,can be labeled as possible VD symptomatology. For example,a radiologist might report “mild diffuse periventricular white matter T2/FLAIR hyperintensity with scattered hyperintense flair signal in the deep and subcortical white matter,” for a scan with a rating of 3 for DWMHs on the Fazekas scale,associated with a score of 24 on the Beck Depression Inventory,Second Edition (BDI-II) and 23 on the Hamilton Depression Rating Scale(HAM-D),and evidence of poor neuropsychological performance. In this case,it is possible that the diagnosis is VD. Table 1 provides additional examples of such scenarios that are described below.
Case reports
Figure3 shows brain scans from a patient who was diagnosed with VD. Patient 1 is a 56-year-old African American female with a HAM-D score of 17 (moderate depression) and a BDI-II score of 12 (minimal depression). She had a Cumulative Illness Rating Scale - Geriatrics (CIRS-G) score of 8. The CIRS-G assesses the severity of disorders in a geriatric population and consists of 14 medical problems,with each problem rated from 0 being no problem to 4 being extremely severe,for a total score range of 0 to 56. She scored a 29 out of 30 on the Mini Mental Status Exam (MMSE),indicating intact mental status. Her performance on a task of processing speed was in the low average range,while performance on a task of cognitive flexibility was in the impaired range. Her performance on the Stroop Test,as compared to the sample mean from the VD research study she was involved in,was in the borderline range,indicating poorer response inhibition than the sample. Using the Fazekas scale,the MRI scan was rated a DWMH score of 2 and a PVWMH score of 3.The radiologist's comment for this patient is as follows: “Multifocal white matter T2/FLAIR hyperintense lesions,the largest of which are located in the left corona radiata and left centrum semiovale,some of which have T1 hyperintensity,most consistent with a condition of microvascular ischemic disease.”
Patient 2 is an 81-year-old Caucasian male with a HAM-D score of 22 (severe depression) and a BDI-II score of 22 (moderate depression). He had a CIRS-G rating of 5 and intact mental status (MMSE = 29). His performance on tasks of processing speed and cognitive flexibility was in the average range,and his performance on a task of response inhibition was in the low average range. Using the Fazekas scale,the MRI scan was rated a DWMH score of 3 and a PVWMH score of 3. The radiologist's comment for this patient is as follows: “Moderate periventricular and deep white matter foci of hyperintense FLAIR signal,more confluent in the right greater than left frontal lobe,most likely due to microvascular ischemia in this age group,accounting for concomitant cerebral/cerebellar atrophy and ventricular dilatation.”
Patient 3 is a 77-year-old African American female with a HAM-D score of 20(severe depression) and a BDI-II score of 14 (mild depression). She had a CIRS-G rating of 6 and intact mental status (MMSE = 29). Performance on a task of processing speed was in the low average range,while performance on a task of cognitive flexibility was in the average range. Performance on a task of response inhibition was impaired. The MRI scan was rated a Fazekas DWMH rating of 2 and a PVWMH rating of 3,and the radiologist commented “Scattered deep and subcortical punctate foci of hyperintense FLAIR signal in the bilateral frontal,parietal and temporal lobes. Nonspecific patterns likely to represent sequela of migraineheadaches,Lyme infection,vasculitis or microvascular ischemia.”
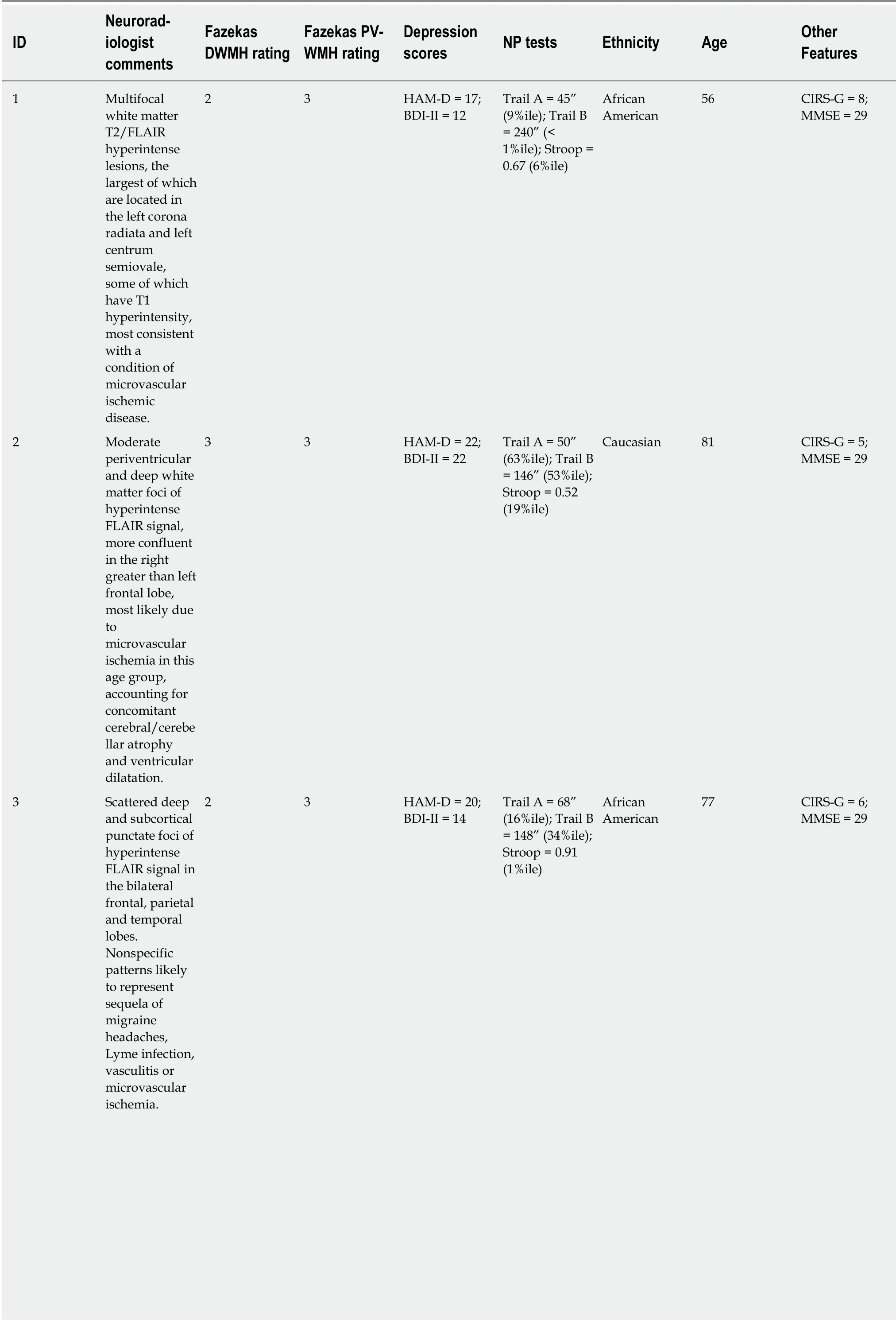
Table1 Vascular depression profiles
DWMH: Deep white matter hyperintensities;PVH: Periventricular hyperintensities;HAM-D: Hamilton Rating Scale for Depression;BDI-II: Beck Depression Inventory,2nd edition;NP: Neuropsychological;%ile: Percentile;CIRS-G: Cumulative Illness Rating Scale - Geriatrics;MMSE: Mini Mental Status Exam.
Patient 4 is a 65-year-old African American male with a HAM-D score of 25 (very severe depression) and a BDI-II score of 21 (moderate depression). He had a score of 6 on the CIRS-G and intact mental status (MMSE = 29). On tasks of processing speed and cognitive flexibility,performance was in the impaired range,while on a task of response inhibition,performance was in the average range. Fazekas ratings of 3 were given for both DWMH and PVWMH. The radiologist commented “Diffuse periventricular and deep white matter foci of hyperintense FLAIR signal in the bilateral frontal parietal and temporal lobes,some of which presenting an ovoid shape perpendicular to the long axis of the lateral ventricle. Primary consideration is multiple sclerosis in the appropriate clinical setting. Other possibilities include microvascular ischemia,vasculitis or prior infection.”
Patient 5 is a 53-year-old African American female with a HAM-D score of 41 (very severe depression) and a BDI-II score of 43 (severe depression). She had a score of 5 on the CIRS-G and intact mental status (MMSE = 28). Performance on a task of processing speed was in the average range while performance on a task of cognitive flexibility was in the impaired range. Performance on a task of response inhibition was in the low average range. The MRI scan was rated a Fazekas DWMH rating of 2 and PVWMH rating of 2. The radiologist noted “Mild periventricular and pontine white matter hyperintense FLAIR signal;additional punctate foci of hyperintense FLAIR in the deep and subcortical frontal-parietal white matter. Nonspecific likely due to microvascular ischemia,migraine headaches,or vasculitis.”
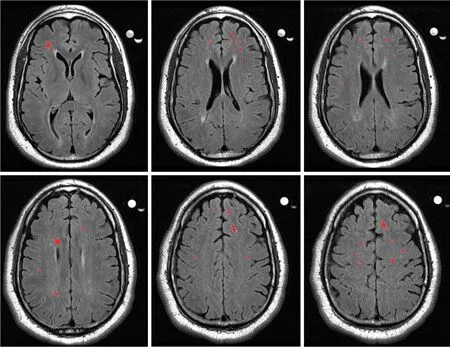
Figure3 Axial slices from a magnetic resonance imaging scan of a vascular depression patient.
All of the above cases represent patients who should be considered for a diagnosis of VD. All patients had elevated depression indices and neuropsychological test performance often showed evidence of impairment in areas of executive function. All patients also had intact mental states and relatively low ratings of general illness severity. Combined with Fazekas ratings of 2 and 3,the presentations indicate VD as a possible diagnosis. As such,treatments should be selected with this diagnosis in mind and vascular depression should be included in probable differential diagnoses.
In addition to the case series,Table 2 depicts primary and secondary features of VD for radiologists to have a reference guide for creating a database of potential VD cases.Importantly,radiologists will need access to information about patients beyond neuroanatomical scans in order to form such a database. Such information as described in Table 2 should be provided in referral questions and records from psychiatrists and psychologists.
CONCLUSION
As the vascular depression hypothesis becomes more refined,the need to identify and treat this population intensifies. In fact,Gonzalezestimated that approximately 2.64 million American adults aged 50 years or older meet criteria for VD.Furthermore,Gonzalezfound that in adults with lifetime major depression,approximately 22% of participants met criteria for the VD subtype. Combined with the increasing aging population,this high incidence rate depicts the importance of accurate identification of these patients.
White matter hyperintensities have been shown to have clinical importance in VD,as they predict a poor response to treatment and increased relapse rate,but their cause remains unclear. Interventions to slow lesion progression may ultimately be able to improve depression outcomes. With accurate identification early on in this disorder,treatment options other than antidepressants can be evaluated,since antidepressants are often not effective in VD patients. Alternative treatment options should be considered,such as those that target frontostriatal and planning/organization networks. Psychosocial treatments such as Problem Solving Therapy have been effective in helping depressed older adults with executive dysfunction.Cognitive remediation strategies that target these areas may also prove to be effective.For example,in a preliminary study,Morimotoinstituted a frontostriataltargeted computerized cognitive remediation program with depressed older adult antidepressant non-responders and found that depression scores were significantly lower after four weeks for those with more executive dysfunction.
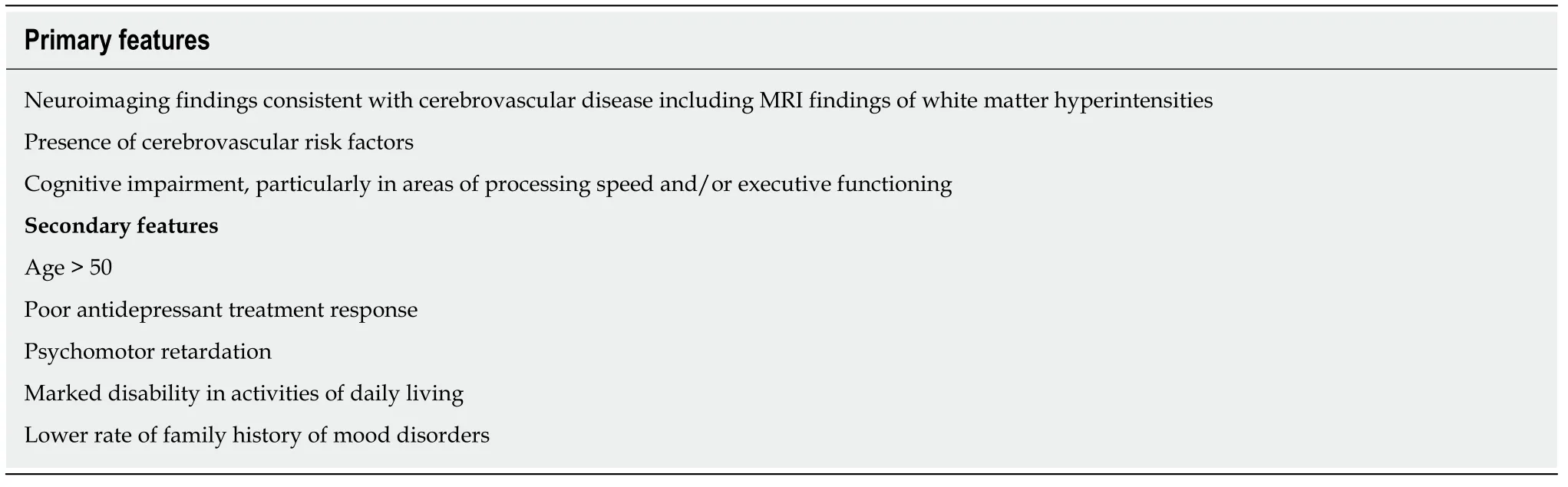
Table2 Primary and secondary features of vascular depression
As imaging techniques become increasingly sophisticated,WMHs will be able to be measured with greater accuracy than ever before. However,it is unlikely that this will replace semi-quantitative scoring systems in the foreseeable future. For research purposes,it would be beneficial for there to be a standardized way of scoring VD brains to improve replicability.
The importance of white matter hyperintensities in VD also indicates an increased need for the assistance of neuroradiologists in identifying these potential patients. Not only is it crucial for neuroradiologists to consider this diagnosis when evaluating MRI scans of older depressed adults,but it is important to increase the involvement of psychiatrists and psychologists in imaging decisions. The access to neuroimaging needs to be improved such that mental health providers are able to request neuroimaging. Additionally,it would be helpful for mental health providers to inform neuroradiologists of each patient's symptomatology,so that neuroradiologists have background information that may influence possible diagnoses when evaluating imaging. As imaging techniques become more advanced,it becomes more likely that imaging will be brought into the scope of psychiatry and psychology,especially with depressive disorders. The use of imaging within psychiatry and psychology has the power to influence the management of symptoms in a critical way. Psychiatrists,psychologists,and neuroradiologists can and should work together,especially when interpreting subtle white matter changes on MRI. Both lesion severity and location should be considered important pieces of information,until such time when one is delineated as being more influential than the other for treatment or disease progression purposes. In the assessment of an older adult patient who has depression,VD should be included as a rule-out for psychiatrists,psychologists,and neuroradiologists. With clinical,neuropsychological,and radiological indicators that separate vascular depression from other depressive disorders,it is critical that patients be evaluated for this disorder.