Cardiovascular disease and COVlD-19, a deadly combination: A review about direct and indirect impact of a pandemic
Rafael Vidal-Perez, Mariana Brand?o, Michal Pazdernik, Karl-Patrik Kresoja, Myriam Carpenito, Shingo Maeda, Rubén Casado-Arroyo, Saverio Muscoli, Janine P?ss, Ricardo Fontes-Carvalho, Jose Manuel Vazquez-Rodriguez
Rafael Vidal-Perez, Jose Manuel Vazquez-Rodriguez, Servicio de Cardiología, Unidad de Imagen y Función Cardíaca, Complexo Hospitalario Universitario A Coru?a Centro de Investigación Biomédica en Red-Instituto de Salud Carlos III, A Coru?a 15006, Spain
Mariana Brand?o, Ricardo Fontes-Carvalho, Department of Cardiology, Centro Hospitalar de Gaia, Gaia 4400-020, Portugal
Michal Pazdernik, Intensive Care Unit, Department of Cardiology, Institute for Clinical and Experimental Medicine Prague, Prague 14021, Czech Republic
Karl-Patrik Kresoja, Janine P?ss, Heart Center Leipzig, University of Leipzig, Leipzig 04289,Germany
Myriam Carpenito, Unit of Cardiac Sciences, Department of Medicine, Campus Bio-Medico University of Rome, Rome 00128, Italy
Shingo Maeda, Arrhythmia Advanced Therapy Center, AOI Universal Hospital, Kawasaki 210-0822, Japan
Rubén Casado-Arroyo, Department of Cardiology, H?pital Erasme, Université Libre de Bruxelles, Brussels 1070, Belgium
Saverio Muscoli, Unit of Cardiology, Policlinico Tor Vergata, Rome 00133, Italy
Ricardo Fontes-Carvalho, Department of Surgery and Physiology, Faculty of Medicine of the University of Porto, Porto 4200-319, Portugal
Abstract Coronavirus disease 2019 (COVID-19) is known to present with respiratory symptoms, which can lead to severe pneumonia and respiratory failure. However,it can have multisystem complications such as cardiovascular manifestations. The cardiovascular manifestations reported comprise myocarditis, cardiogenic shock,arrhythmias, pulmonary embolism, deep vein embolism, acute heart failure, and myocardial infarction. There is also an indirect impact of the pandemic on the management of cardiovascular care that has been shown clearly in multiple publications. In this review, we summarize the deadly relation of COVID-19 with cardiovascular events and the wider impact on several cardiovascular care areas by the pandemic situation
Key Words: COVID-19; Cardiovascular diseases; Pandemic; Heart failure; Telemedicine; Prognosis
lNTRODUCTlON
The complete impact of the pandemic has been much greater than what is indicated by reported deaths due to coronavirus disease 2019 (COVID-19) alone. Indirect effects of the pandemic have been present on cardiovascular disease management and could justify partially the excess of death related with COVID-19[1].
The prior presence of cardiovascular disease is an important risk factor for a severe clinical course of COVID-19 and is associated with unfavorable outcomes[2,3]. Furthermore, COVID-19 may aggravate underlying heart disease and is frequently worsened by cardiovascular complications, such as thromboembolic events, malignant arrhythmia, and myocardial injury[4]. COVID-19 also has been associated with a direct damage of the cardiovascular system[5].
In this review, we will focus on the direct and indirect impact of the pandemic in relation with cardiovascular diseases to show that cardiovascular disease and COVID-19 really were a deadly combination.
THROMBOEMBOLlC COMPLlCATlONS
Arterial and venous thromboembolic events are frequently observed in COVID-19 patients and contribute to increased morbidity and mortality[4,6].
Venous thrombotic events
The incidence rates of venous thrombotic events (VTE) reach more than 30% in cohorts of critically ill patients despite pharmacological prophylaxis[7]. As evidence of the activated coagulation system, Ddimer plasma levels are elevated in a relevant proportion of COVID-19 patients, associated with an adverse outcome[8]. Numerous randomized controlled trials have evaluated the role of therapeutic doses of heparin in reducing VTE events or mortality in patients hospitalized due to COVID-19. In the intensive care unit (ICU) scenario, these studies showed that heparin at therapeutic doses did not reduce mortality but may be associated with a higher risk of bleeding events; consequently, this approach is not recommended. According to the current guidelines, hospitalized COVID-19 patients should receive at a minimum routine thromboprophylaxis. Therapeutic-dose heparin should be used for hospitalized COVID-19 patients who have a D-dimer level above the upper limit of normal, require low-flow oxygen, and have no increased bleeding risk. In the patients receiving ICU level of care, prophylacticdose heparin is recommended[9].
Arterial thrombotic events: Stroke and acute myocardial infarction
COVID-19 is an independent risk factor for the occurrence of ischemic stroke, with a higher risk in patients with a severe clinical course[10]. The reported stroke rate of COVID-19 patients is approximately 1%. Notably, patients with COVID-19 seem to have an increased risk for cryptogenic and large vessel stroke[4].
Furthermore, COVID-19 has been descried as a relevant risk factor for the development of acute myocardial infarction (AMI)[11]. A large fraction of patients presenting with AMI and accompanying severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection has type II MI caused by the primary infection inducing respiratory and/or hemodynamic derangement. It remains controversial whether SARS-CoV-2 can trigger type I MI; the potential underlying mechanisms might be cytokinerelated plaque instability, immune-thrombosis, and endothelitis[4,12]. Patients presenting with SARSCoV-2 infection and concomitant ST elevation myocardial infarction (STEMI) have a high thrombus burden, a high risk for stent thrombosis, and an increased risk for a poor outcome[13]. Importantly, the COVID-19 pandemic should not compromise timely reperfusion in STEMI, and management of patients with non-ST-segment elevation acute coronary syndromes (ACS) should be guided by clinical risk stratification[14].
TAKOTSUBO SYNDROME
Through the COVID-19 pandemic, a substantial increase in the incidence rate of Takotsubo syndrome was observed[15]. Notably, in one study, the majority of patients presenting with Takotsubo syndrome tested negative for SARS-CoV-2, potentially implying an increased level of stress in the general population due to the public health measure to reduce transmission rates (social distancing rules, selfisolation, and quarantine), economic stress, and fear of infection[4,15].
ACUTE HEART FAlLURE
Progressive dyspnoea is both the hallmark symptom of acute heart failure (AHF) as well as severe COVID-19 and distinguishing these entities is challenging, as up to 12% of hospitalised COVID-19 patients might have an established diagnosis of chronic heart failure[16]. Natriuretic peptides might also be elevated in COVID-19 patients even in the absence of left ventricular systolic impairment, proving another challenge in differentiating both entities[14,17]. In line with this, COVID-19 might both trigger AHF in patients with a known history of heart failure as well as lead to a first episode of hospitalization in patients with occult heart failure[18]. Whether these factors are causative or just coincident is currently within the scope of scientific research. However, several factors induced by COVID-19 might be contributing to mechanisms of AHF such as acute myocardial injury defined as increase of circulating troponin levels (observed in 8% to 15% of COVID-19 patients), which has been described to be associated with disease severity[19]. Besides unspecific myocardial injury, the myocardium might also be deteriorated due to COVID-19 associated myocarditis, whereas both direct cardiomyocyte infection and autoimmune myocarditis have been described[20]. Acute respiratory distress syndrome(ARDS), hypoxemia, renal failure, volume expansion, increased sympathetic drive, fever, and systemic inflammatory response syndrome, factors that are commonly present in severe respiratory disease,might further induce or aggravate heart failure[21].
While AHF rates have consistently been reported to decline worldwide, there was an increase in symptom burden as well as a higher in-hospital mortality rate as compared to historical data observed during the COVID-19 pandemic[14,19,22,23]. Among patients with known heart failure, one third of patients hospitalised with COVID-19 and up to 50% of those that developed AHF died within the inhospital stay[8]. Patients with heart failure and COVID-19 that had to be admitted to an ICU had an even higher mortality rate of up to 75%[16].
Besides left sided heart failure, acute right heart failure, which might occur secondary to acute pulmonary hypertension or ARDS, has been described in patients with COVID-19[24]. Even in the absence of manifestations of right heart failure, right ventricular dysfunction appears in nearly 15% of patients with COVID-19 and might contribute to impaired outcomes, irrespective of heart failure state[25]. Moreover, there has been recent data that patients following SARS-CoV-2 infection are at increased risk of developing cardiovascular disease even after the acute phase of infection often referred to as“l(fā)ong COVID”[26].
EFFECTS OF THE COVlD-19 PANDEMlC ON ACUTE CARE OF PATlENTS WlTH CARDlOVASCULAR DlSEASE
In addition to the increased risk of an adverse outcome of SARS-CoV-2 infection and to the cardiovascular effects of COVID-19, patients with cardiovascular disease suffer from indirect consequences of the pandemic. Profound adaptations of health care systems were necessary to cope with the high number of severely ill patients with SARS-CoV-2 infection. This included a deferral of a substantial number of elective procedures and affected the acute care of patients with cardiovascular diseases[27]. The New York Times asked in April 2020: “Where have all the heart attacks gone?”Multiple reports from different European countries, the United States, and China show a marked reduction in hospital admissions due to ACS[28-32]. A meta-analysis of 27 international studies corroborated these results, showing a 40%-50% reduction of hospital admissions due to ACS[33]. The interval between symptom onset and admission to the hospital was increased most likely because patients waited longer until they called the emergency services. An observed increase of the door-to-devicetimes[34,35] might be partly attributable to the recommendations regarding protective measures for the staff as well as adapted reperfusion strategies including fibrinolysis in STEMI and conservative strategies in non-STEMI[36,37]. Hospital admissions due to other acute cardiovascular conditions were also reduced during the pandemic[35,38]. Reports on the effects of the pandemic on in-hospital mortality of AMI are heterogeneous[27]. Some studies describe increased rates of mortality; others show no difference[29,34,39,40]. The above-mentioned meta-analysis showed an increased AMI mortality from March to May 2020[33]. The observed increase in prehospital deaths and out-of-hospital cardiac arrests implies a negative impact of the pandemic on total mortality rates of AMI[41,42]. Table 1 gives an overview on potential causes for chances in acute cardiac care during the COVID-19 pandemic.

Table 1 Potential causes for changes in acute cardiac care during the coronavirus disease 2019 pandemic
MYOCARDlTlS
COVID-19-associated myocardial injury, defined as serum troponin level above the 99thpercentile of the upper reference limit, was reported from the early days of the pandemic[43]. In several studies,myocardial injury was common among COVID-19 patients, with a very wide prevalence ranging from 8%-62% according to the study and the definition used[43,44]. Nevertheless, almost all studies have shown that these patients had a worse prognosis[44].
Interestingly, even after 2 years of the onset of the COVID-19 epidemic, the pathogenesis of myocardial injury remains unknown. Numerous authors have stated that it may be largely attributable to prominent systemic inflammation, rather than to direct viral infection of the heart[43,44]. This is concordant with the pathophysiology of severe forms of COVID-19, where a profound proinflammatory state, the so-called “cytokine storm”, is thought to take place[45]. In a systematic review comprising nearly 200 COVID-19 patients submitted to cardiac magnetic resonance imaging, myocarditis was the most common imaging diagnosis (40.2%). Evidence of diffuse myocardial edema (T1 and T2 mapping abnormalities) and fibrosis (late gadolinium enhancement) were amongst findings in these patients.
However, the ability of SARS-CoV-2 to directly cause cardiomyocyte infection and damage remains controversial. According to the current definition of myocarditis, proposed by the European Society of Cardiology (ESC) Working Group on Myocardial and Pericardial Diseases, a definitive diagnosis can only be made when a viral genome is proven in endomyocardial specimens along with the histological findings of active myocarditis[46]. In April 2020, a group from Padua University reported the first case of biopsy-proven viral myocardial involvement in a COVID-19 patient presenting with cardiogenic shock[47]. However, to this date, there have been limited reports with pathological evidence of COVID-19 direct myocardial invasion. The potential for long-term evolution into forms of inflammatory cardiomyopathy remains also unclear.
More recently, with the large-scale use of several COVID-19 vaccines, the attention shifted to COVID-19 vaccination-related myocarditis. Despite not being reported as an adverse event in the first vaccine clinical trials, several cases were observed soon after vaccination campaigns began, particularly with mRNA technology vaccines. In May 2021, the Centers for Disease Control and Prevention released a report stating a possible association between COVID-19 vaccination and myocarditis, regarding the BNT162b2 (Pfizer-BioNTech) and the mRNA-1273 (Moderna) vaccines[48]. Later, an analysis of 2.5 million vaccinated people from Israel expected the incidence of post-vaccination myocarditis to be 2.13 cases per 100000 vaccinated persons[49]. In this cohort of patients who received the BNT162b2 mRNA vaccine (Pfizer-BioNTech), the highest myocarditis incidence was among young male patients, and after the second vaccine dose[49]. Another large English study showed similar findings, namely, an increased risk of myocarditis in patients who received the 2nddose, and in those aged below 40[50]. Across published reports, vaccine-associated myocarditis was mostly a self-limiting disease of mild to moderate severity[50,51]. It has been hypothesized that post-vaccination myocarditis, similarly to COVID-19 myocarditis itself, can result from immune-mediated, virus-independent immunopathologic mechanisms[50,52].
Although this topic gathered intense attention from the social media, it is known that SARS-CoV-2 infection in non-vaccinated people carries a much greater risk of hospitalization and death than the vaccine associated risks[51]. Vaccines have proved to be highly effective at preventing symptomatic and severe disease, and remain, to this moment, the most powerful instrument to halt the effect of this dramatic pandemic on public health and social and economic domains.
CARDlAC ARRYTHMlAS
Cardiac arrhythmias may be not only the consequence of direct effects of SARS-CoV-2 infection but also the effects of the adverse reactions to medications used for the treatment of the infection and systemic illness (Figure 1). A metanalysis of 17 retrospective cohort studies of almost 6000 patients showed that the incidence for cardiac arrhythmias (Table 2) was 9.3%[53,54]. Table 3 describes the main mechanism of arrhythmogenicity in this setting[55].

Figure 1 Proposed mechanism of cardiac arrhythmias described in patients with SARS-CoV-2 infection.
Atrial fibrillation
Atrial fibrillation was the most frequent cardiac arrhythmia detected in patients with SARS-CoV-2 infection. Virus-induced cardiac injury in the context of myocarditis, hypoxemia, systemic inflammatory response, and autonomic dysfunction are some of the mechanism implicated in the pathogenesis of ventricular fibrillation (VF) in this setting.
Ventricular arrhythmias
Ventricular arrhythmias (ventricular premature complexes, non-sustained and sustained ventricular tachycardia, polymorphic ventricular tachycardia, and ventricular fibrillation) may occur in the same context of the previous described AF, but also due to the proarrhythmic effects of COVID therapies.Ventricular arrhythmogenicity can be enhanced by acidosis, electrolyte disturbances, fever in Brugada patients, and pre-existing or acquired QT prolongation and induced by drugs.
In a retrospective cohort study of more than 1000 patients having a cTn level measured on admission,arrhythmias developed in 44 of the 170 (25.9%) that showed a high cTn level on admission, including six patients with ventricular tachycardia (VT) or VF. The mortality was 100% in this population[56].
Another report compared all the consecutive out-of-hospital cardiac arrests in 2 mo after the first documented case of COVID-19 in a region of Italy with those which occurred in the same time frame in 2019. The cumulative incidence of out-of-hospital cardiac arrest was 21 cases/100000 inhabitants, with a 52% rise as compared with the previous year (P< 0.001)[57]. Table 4 describes the main measures to prevent ventricular arrhythmias[2].
Drug-induced prolongation of QTc interval
Several agents used for potential prophylaxis and for treating SARS-CoV-2 infection prolong the QT interval and lead to polymorphic VT in the form of torsades de pointes (TDP) (Table 5)[2]. Some simple measures have been proposed to avoid TDP, like avoiding QT prolonging drugs in patients with baseline QTc > 500 ms or with known long QT syndrome, when QTc increases to > 500 ms or if QTc is prolonged by > 60 ms compared to baseline measurement, avoiding drugs of uncertain clinical effect against COVID-19 in patients with known risk factors such as prolonged QTc, and monitoring and avoiding hypomagnesemia, hypokalaemia, concomitant use of certain QT prolonging antiarrhythmic drugs, including class IA (procainamide and quinidine) and class III (sotalol and amiodarone), or bradycardia.

Table 2 Cardiac arrhythmias described in patients with severe acute respiratory syndrome coronavirus-2 infection[53]

Table 3 Mechanisms of arrhythmogenicity[55]

Table 4 Measures to prevent ventricular arrhythmias[58]
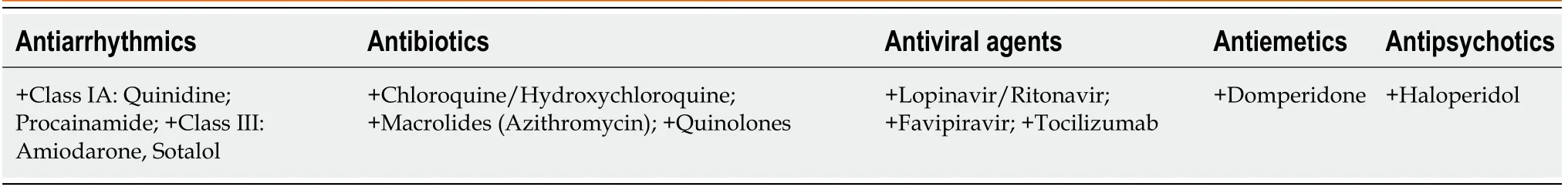
Table 5 QT prolonging drugs to avoid during severe acute respiratory syndrome coronavirus-2 infection[58]
Acute myocardial injury
A meta-analysis analyzing more than 4600 patients showed that patients with newly occurring arrhythmias and cardiac injury were at higher risk of requiring ICU admission or developing severe disease (relative risk [RR]: approximately 13,P< 0.001)[58].
Sinus tachycardia
Sinus tachycardia is the most frequent heart rhythm disturbance during the acute infection, due to fever,respiratory insufficiency, hemodynamic compromise, anxiety, and pain, among others. In the chronic context, the origin of sinus tachycardia is mainly due to physical deconditioning and autonomic dysfunction[59].
Conduction disturbances
A study showed that the presence of atrial premature contractions, right bundle branch block, or intraventricular block increased the odds of death[60].
Implantation of cardiac implantable electronic devices
A German study showed that the pandemic was associated with an overall decline of device implantation rates of -2.6%, with a peak of almost -23%[61]. This situation was limited in time. The COVID-19 pandemic has led to a significant increase in the use of remote monitoring of cardiac implantable electronic devices[62].
CHRONlC CORONARY SYNDROME
Other pre-existing inflammatory conditions such as chronic coronary syndrome (CCS) may be associated with worse clinical outcomes in the context of COVID-19. In CCS, the cytokine storm triggered by SARS-CoV-2 infection may favour the rupture of a silent atheromatous plaque, leading to acute coronary syndrome and a sudden worsening of the patient's clinical condition[63].
CCS patients are generally at low risk of acute cardiovascular events, so diagnostic and/or interventional procedures can be deferred in most cases. In these patients, medical therapy should be optimized and/or intensified with the help of telemedicine. Remote clinical monitoring should be ensured to reassure patients and to detect possible changes in clinical status that may require hospitalization in selected patients with a high risk profile[14].
Therefore, during the first phase of the pandemic, it was necessary to continue follow-up in these patients, but with some restrictions.
Non-steroidal anti-inflammatory drugs may worsen the course of community-acquired pneumonia;on the contrary, their negative involvement in exacerbation of SARS-CoV-2 infections is not yet known.The possible effects of chronic aspirin therapy are not clearly understood. However, aspirin has only a very limited anti-inflammatory effect at the low dose administered in CCS. Therefore, CCS patients should not discontinue aspirin for secondary prevention[64].
In patients admitted with influenza or pneumonia, statin therapy has been variably associated with favorable outcomes. Alternatively, patients with COVID-19 have been reported to develop elevated liver enzymes or severe rhabdomyolysis and it may be advisable to temporarily suspend statin therapy[65,66].
During the initial phase of the COVID-19 pandemic, asymptomatic visits of patients with suspected CCS were often deferred as financial resources were allocated to the pandemic. In symptomatic patients with suspected coronary artery disease and a pre-test probability of 5%-15%, functional imaging examinations to detect myocardial ischaemia such as coronary computed tomography angiography were preferred to other imaging techniques such as stress echocardiography to avoid close contact between patients and medical staff[67].
After the initial phase, some changes were established in some local protocols, allowing cardiac testing of patients wearing facial masks, and this approach showed to be feasible, reaching the same levels of effort as in the prepandemic period for treadmill tests[68].
CHRONlC HEART FAlLURE
Association between SARS-CoV-2 infection and chronic heart failure (HF) may manifest as follows: (1)Patients with HF are at increased risk for severe and complicated course of COVID-19; (2) SARS-CoV-2 infection can exacerbate chronic HF; and (3) The COVID-19 pandemic is linked with dramatic changes in the delivery of outpatient care of HF patients
Patients with SARS-CoV-2 infection and pre-existing HF are more likely to be critically ill, with increased rates of ICU admission, renal replacement therapy, and mechanical ventilation[69]. Preexisting HF represented an independent risk factor for mortality during COVID-19 hospitalization, with an adjusted odds ratio of 1.88 (95% confidence interval: 1.27-2.78)[70]. A large retrospective cohort study in United States veterans in the ambulatory setting testing positive for SARS-CoV-2 described that patients with COVID-19 and previously diagnosed HF had a greater risk of 30-d mortality and hospital admissions[71]. Interestingly, most of the clinical presentations of COVID-19 on top of advanced HF were dyspnoea and worsening of haemodynamic status instead of fever and other signs and symptoms of infection[72].
COVID-19 may cause or worsen HF through multiple mechanisms including myocardial ischemia or infarction, activation of the sympathetic nervous system, neurohormonal activation precipitating volume retention, elevations in pulmonary pressures, myocarditis, pulmonary embolism, stress cardiomyopathy, and inflammation leading to myocardial depression. The above mentioned mechanisms play a pivotal role and may subsequently lead to arrhythmias, cardiogenic shock, and/or sudden cardiac death[69,18].
Furthermore, it is not known whether the clinical course of COVID-19 differs depending on the left ventricular ejection fraction or background medication[73]. SARS-CoV-2 uses the angiotensinconverting enzyme (ACE)-2 receptors for cell entry and early data suggested that ACE inhibitors(ACEIs) and angiotensin receptor blockers (ARBs) may upregulate ACE2, hypothetically increasing susceptibility to infection[74]. However, there is no clinical evidence linking ACEI/ARB treatment and susceptibility to infection or clinical course. Moreover, the available data do not support the discontinuation of ACEI/ARB in HF patients with COVID-19, which could increase the risk of death[75].Consequently, it could be recommended that HF patients continue to take all prescribed guidelineappropriate medications (including ACEI, ARB, or sacubitril/valsartan) regardless of COVID-19[76].Pneumococcal and influenza vaccination, as well as COVID-19 vaccination, when available, should be considered in patients with HF[77].
During COVID-19 pandemics, healthcare institutions have been forced to reconfigure the day-to-day routine ambulatory care. Adoption of restraint measures as an indirect impact of COVID-19 pandemics resulted in decreased hospital admissions for AHF and reduced number of self-referred AHF patients[78,79]. Altered medical care delivery was also confirmed in the multicentre, multinational PCHFCOVICAV registry, which demonstrated that COVID-19 impacted referral and hospitalizations of patients with acute HF and that HF was linked with a high mortality[80].
With an aim to diminish COVID-19 transmission during unnecessary hospitalizations of HF patients,and to maintain a healthy hospital workforce, medical facilities have broadly transitioned to noncontact care delivery methods for out-patient clinical care[81]. Several studies confirmed that this approach was able to keep a low proportion of admissions due to HF decompensation, without an increase in mortality. Results of these studies supported the implantation of telehealth outpatient visits in patients with HF and their safe incorporation into clinical practice[82].
lMPACT ON VALVULAR HEART DlSEASE
Over the past decade, structural cardiac intervention has been increased worldwide, particularly transcatheter aortic valve implantation (TAVI), transcatheter mitral edge-to-edge repair (TEER), left atrial appendage closure (LAAC), atrial septal defect (ASD) closure, and patent foramen ovale (PFO)closure. This increase in structural cardiology is due to progressive improvements in technology,scientific support from several randomized controlled trials, and life expectancy.
The global COVID-19 pandemic profoundly impacted the treatment of patients eligible for coronary and structural cardiology interventions, as many hospitals had to adjust their internal organization and reallocate economic resources[83].
Structural interventions are usually elective and rarely performed in urgent cases as they require careful clinical and imaging examination such as CT and transthoracic (TT) or transoesophageal (TE)echocardiography. Hospitals changed their management, especially for all procedures requiring ventilators or intensive care. This forced restructuring led to significant constraints, delays, and, in some cases, deletion of procedures, especially in the first phase of the pandemic. TAVI, TEER, and LAAC procedures were reserved for urgent or highly symptomatic patients, while PFO closure, a procedure performed in the elective regime, was almost entirely suspended[84].
In addition, valvular heart disease (VHD) can exacerbate the course of COVID-19 and complicate treatment. An excess of mortality has been reported, particularly in patients with VHD infected with SARS-CoV-2; of 136 elderly patients with severe VHD (54% with aortic stenosis), 84.6% were treated conservatively, and the mortality rate was 41.8% after 30 d[85].
The first peak of the pandemic in England led to a considerable decrease in surgical valve interventions, 73%-76% for aortic valve replacement and 84%-85% for mitral valve replacement, while TAVI was less affected, with 35% and 18% decreases in April and May 2020, respectively[86].
The priority of valve interventions should therefore weigh the need for treatment, the immediate and short-term prognosis, available resources, and the risk to patients and healthcare professionals (HCPs)of hospital-acquired infections.
The ESC, the Society of Cardiovascular Angiography EuroIntervention and Interventions, and the Canadian Association of Interventional Cardiology have published their position statements on the management of structural heart surgery during the pandemic COVID-19[14,87,88].
As the pandemic continues, many centers have adopted a “minimalist” approach to TAVI, which is next day discharge (NDD) following transfemoral TAVI. NDD is a safe strategy for both balloonexpandable and self-expanding implants in selected cases[89].
It allows rapid discharge and avoids the risk of COVID-19 transfer to the patient in the hospital while ensuring patient treatment and medical care at a time of limited resources. NDD is unfortunately not performed in many centers, and for structural procedures, there is likely to be a long waiting list and a high burden for patients with symptomatic aortic stenosis when the pandemic recedes. Long waiting times can have a significant social and clinical impact, even in patients initially considered being at low risk of cardiovascular events. A possible solution should be to avoid standard referral to the ICU in centers with a high volume of procedures and expertise of surgeons using NDD, reserving it only for necessary cases, with all post-procedural care provided in a cardiovascular ward[90].
Treatment of mitral regurgitation (MR) differs according to aetiology and presentation. Chronic primary MR is usually well tolerated. In contrast, secondary MR is more variable and can lead to unstable HF syndromes that do not respond to medical treatment, especially in acute infections.Therefore, in the context of the pandemic, priority should be given to the treatment of acute primary MR complications (AMI or IE) and those with severe primary or secondary MR, which are symptomatic despite optimal medical therapy (OMT) and require hospitalization[91].
TEER requires general anesthesia (unlike transfemoral TAVI) and a longer TE echocardiograpy,exposing healthcare workers to the risk of COVID-19 transmission.
In contrast to patients affected by severe and symptomatic aortic stenosis, the majority of patients with severe MR can be managed by OMT, and indeed TEER has been deferred or reserved only for special cases during the pandemic. A web-based survey sent to EAPCI members from April 1 to 15, 2020 showed that TEER was discontinued in 73% of cases. A web-based survey sent to EAPCI members from April 1 to 15, 2020 showed that TEER was discontinued in 73% of cases[92].
Some changes in the classical organization of procedural protocols have been proposed to manage TEER better and avoid long waiting lists, especially in the postoperative phase. Same-day discharge(SDD) is increasingly practiced in larger centers, as shown by an observational study in which 89 patients who had an uncomplicated MitraClip inserted under moderate conscious sedation were discharged the same day without significant complications[93].
Chowdhuryet al[94] developed a SDD protocol for patients treated during the pandemic by TEER.SDD reduced length of stay, resource utilization, and nosocomial SARS-CoV-2 infection risk. Patients were admitted 1 day before TEER, extubated in the cath lab, transferred to the recovery ward, and treated as outpatients within 2 h; then a TT echocardiogram was performed to assess outcomes and rule out pericardial effusion. If there was no immediate postoperative complication, they were discharged 3-4 h after the procedure. The protocol also included a telephone follow-up the next day and a follow-up at 2 wk and 30 d[94].
A new option for severe mitral regurgitation is transcatheter mitral valve replacement. This is a new and promising technique. Initial case series suggest that it is feasible and can lead to improvement in symptoms[95]. Numerous devices have been suggested in recent years, but unfortunately the use of this treatment has declined dramatically during the pandemic.
Other structural heart procedures, such as closure of PFO and ASD and LAAC, were unaffected in 9%, while complete cessation of activities was reported in 79%[92].
Two years after the pandemic, we are returning to normality, mainly due to the spread of the vaccine.Nevertheless, we have learned lessons from the first months of the pandemic that we are currently applying, such as avoiding extended hospital stays and promoting early discharge, avoiding intensive care unless absolutely necessary, and focusing on frequent follow-up.
lMPACT ON CARDlOVASCULAR lMAGlNG
Cardiovascular imaging (CVI) plays a pivotal role in the diagnostic pathway of both acute and chronic cardiovascular disease. The devastating impact of the COVID-19 pandemic on the treatment of patients with cardiovascular disease extended also to all cardiac imaging modalities, and likely contributed to delayed diagnosis of cardiovascular (CV) disease. Given its key role as a bedside test, and the “close contact” with the patient, echocardiography was the most affected cardiac imaging modality at the beginning[96]. Given the uncertainties of the disease since the beginning of the pandemic, the European Association of Cardiovascular Imaging issued specific recommendations for the use of cardiac imaging in this setting. Recommendations for the use of CVI were limited only to situations where it was likely to substantially change patient management or be lifesaving[96]. At that time, it was proposed that routine follow-up examinations and elective non-urgent procedures should be postponed or even cancelled and that more focused point-of-care examinations should be performed to minimize exposure time[96,97].
The INCAPS COVID survey was designed to assess the impact of COVID-19 on the use of cardiac imaging during the first lockdown. This survey reported a large reduction (45%-69%) in the total number of procedures in March and April 2020 in European countries[98]. Although we know that these numbers steadily recovered from Spring 2020, these results raised concern that the underutilization of CVI testing may have disrupted the implementation of primary and secondary strategies for CV disease prevention[99]. Patients deprived from prescribed CVI examinations could later present with more severe forms of disease, since they were probably not provided with appropriate care that would improve their long-term prognosis.
Furthermore, the COVID-19 pandemic also had a major impact on the well-being of healthcare professionals. A recently reported survey showed that CVI specialists experienced very high levels of stress, anxiety, and burnout during the COVID-19 pandemic, which highlights the psychological burden that these healthcare professionals have confronted and the importance to address proactively this problem[100].
Nevertheless, the pandemic also had some positive impact in cardiovascular imaging. We observed a broadened and more widespread use of pocket echocardiography and especially an increased awareness for the importance of lung ultrasound (LUS). Due to its high sensitivity, bedside availability,and steep learning curve, LUS already had previously well-established value as an important diagnostic and prognostic tool in heart failure and other acute cardiac care scenarios[101]. However, its implementation in the clinical field was accelerated with the pandemic especially because it was also observed that in patients with a diagnosis of COVID-19, LUS could be useful to detect signs of pulmonary involvement, such as pleural thickening, B-lines, or lung consolidation[102]. Although LUS is valuable to diagnose and grade COVID-19 pneumonia, it requires more advanced expertise to recognize typical signs and patterns[102]. However, when used by experienced operators, it can aid clinical decision-making from simple monitoring to mechanical ventilation titration.
In summary, given the wide impact of the COVID-19 on cardiovascular imaging techniques,medium- and long-term consequences may be expected for some patients due to delayed diagnosis and treatment.
TELEMEDlClNE
Today's technology, especially telemedicine, allows following patients with chronic cardiovascular diseases such as CCS and CHF. Some scientific societies focused on this approach due to the COVID-19 pandemic to suggest a better and wider use of telemedicine[103,104].
For known CCS patients, clinical follow-up should be conducted mainlyviatelemedicine. This would allow physicians to address most of the patient's concerns related to continuation or change of medical therapy. Possible occurrence/recurrence of unstable symptoms should be assessed as part of the patient's clinical history to weigh the need for hospitalization and diagnostic tests[14].
Several reports suggest a decrease in hospitalization rates for chronic HF in people without SARSCoV-2 infection during the peak of the pandemic COVID-19 compared to 2019[22].
For the duration of the COVID-19 outbreak, patients with chronic HF should be advised to closely follow protective measures to prevent disease transmission. Outpatients with HF should avoid routine,non-urgent hospital visits, which has led to an increase in telemedicine and remote monitoring work.The increased use of telemedicine has been promoted to minimize infection risk and ensure continuity of care and timely optimization of medical treatment. Several papers have reported the effective use of this technology in medical consultation, treatment adjustment, and follow-up of outpatients HF during the COVID-19 outbreak[105]. Telemedicine has become an important tool for delivering of HF care to ensure continuity of care for the chronically ill while maintaining the safety of patients and HCPs[106].
The changes in hospitals during the pandemic have helped reduce barriers to telemedicine and facilitate its widespread adoption. The chronic heart failure-CePPORT (Canadian e-Platform to Promote Behavioral Self-Management in Chronic Heart Failure Trial) trial highlight an approach to supporting patients with chronic HF[107].
What this change represents for the future of HF management and the provision of HF services in outpatient scenarios worldwide remains warmly debated[108].
Nowadays, far-reaching projects have been proposed for the future management of HF to improve access to care by overcoming transport barriers, the excessive cost of clinical appointments, patient education, and remote home monitoring in more patients tailored ways[18].
CONCLUSlON
The prior presence of cardiovascular disease is an important risk factor for a severe clinical course of COVID-19 and is associated with adverse outcomes. COVID-19 also has been associated with a direct damage of the cardiovascular system.
Although the pandemic seems to be near to its end, an effort must be made to enable the diagnosis of non-COVID-19 conditions that were overlooked during this period as these non-COVID-19 conditions untreated could explain the excess of death during this dramatic period. This should be a priority for policymakers while planning the recovery from these hazardous times. The lessons learnt during this period should serve as preparation for future challenges or impending pandemics that could be again a deadly combination as the COVID-19 was with the cardiovascular diseases.
FOOTNOTES
Author contributions:Vidal-Perez R designed, edited, and wrote the final paper; Brand?o M, Pazdernik M, Kresoja KP, Carpenito M, Maeda S, Casado-Arroyo R, P?ss J, and Fontes-Carvalho R performed the collection of the data and helped in writing the original draft; Vidal-Perez R and Vazquez-Rodriguez JM contributed to the critical revision and editing of the paper; all authors wrote, read, and approved the final manuscript.
Conflict-of-interest statement:All the authors declare that they have no conflict of interest that may affect the content of this article.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Spain
ORClD number:Rafael Vidal-Perez 0000-0001-9944-8363; Mariana Brand?o 0000-0001-9913-0435; Michal Pazdernik 0000-0001-7486-7705; Karl-Patrik Kresoja 0000-0002-8616-6751; Myriam Carpenito 0000-0002-0631-7573; Shingo Maeda 0000-0001-6964-0653; Rubén Casado-Arroyo 0000-0002-3876-6074; Saverio Muscoli 0000-0002-4037-7561; Ricardo Fontes-Carvalho 0000-0003-2306-8393; Jose Manuel Vazquez-Rodriguez 0000-0003-0888-6937.
S-Editor:Wang LL
L-Editor:Wang TQ
P-Editor:Wang LL
 World Journal of Clinical Cases2022年27期
World Journal of Clinical Cases2022年27期
- World Journal of Clinical Cases的其它文章
- lmpact of the COVlD-19 pandemic on healthcare workers’ families
- Transition beyond the acute phase of the COVlD-19 pandemic: Need to address the long-term health impacts of COVlD-19
- Transient ischemic attack after mRNA-based COVlD-19 vaccination during pregnancy: A case report
- latrogenic aortic dissection during right transradial intervention in a patient with aberrant right subclavian artery: A case report
- lnfant with reverse-transcription polymerase chain reaction confirmed COVlD-19 and normal chest computed tomography: A case report
- Successful treatment of stage lllB intrahepatic cholangiocarcinoma using neoadjuvant therapy with the PD-1 inhibitor camrelizumab: A case report
