Nonalcoholic fatty liver disease is associated with worse intestinal complications in patients hospitalized for Clostridioides difficile infection
Yi Jiang,Salil Chowdhury,Bing-Hong Xu,Mohamad Aghaie Meybodi,Konstantinos Damiris,Samanthika Devalaraju,Nikolaos Pyrsopoulos
Yi Jiang,Salil Chowdhury,Mohamad Aghaie Meybodi,Konstantinos Damiris,Samanthika Devalaraju,Department of Medicine,Rutgers New Jersey Medical School,Newark,NJ 07101,United States
Bing-Hong Xu,Liver Center and Center for Asian Health,RWJBH-Saint Barnabas Medical Center,Florham Park,NJ 07932,United States
Nikolaos Pyrsopoulos,Department of Medicine,Gastroenterology and Hepatology,Rutgers New Jersey Medical School,Newark,NJ 07101,United States
Abstract BACKGROUND Nonalcoholic fatty liver disease(NAFLD)has become the leading cause of chronic liver disease with increasing prevalence worldwide.Clostridioides difficile infection(CDI)remains the most common cause of nosocomial diarrhea in developed countries.AIM To assess the impact of NAFLD on the outcomes of hospitalized patients with CDI.METHODS This study was a retrospective cohort study.The Nationwide Inpatient Sample database was used to identify a total of 7239 adults admitted as inpatients with a primary diagnosis of CDI and coexisting NAFLD diagnosis from 2010 to 2014 using ICD-9 codes.Patients with CDI and coexisting NAFLD were compared to those with CDI and coexisting alcoholic liver disease(ALD)and viral liver disease(VLD),individually.Primary outcomes included mortality,length of stay,and total hospitalization charges.Secondary outcomes were in-hospital complications.Multivariate regression was used for outcome analysis after adjusting for possible confounders.RESULTS CDI with NAFLD was independently associated with lower rates of acute respiratory failure(2.7% vs 4.2%,P < 0.01;2.7% vs 4.2%,P < 0.05),shorter length of stay(days)(5.75 ± 0.16 vs 6.77 ± 0.15,P < 0.001;5.75 ± 0.16 vs 6.84 ± 0.23,P <0.001),and lower hospitalization charges(dollars)(38150.34 ± 1757.01 vs 46326.72 ± 1809.82,P < 0.001;38150.34 ± 1757.01 vs 44641.74 ± 1660.66,P < 0.001)when compared to CDI with VLD and CDI with ALD,respectively.CDI with NAFLD was associated with a lower rate of acute kidney injury(13.0% vs 17.2%,P < 0.01),but a higher rate of intestinal perforation(P < 0.01)when compared to VLD.A lower rate of mortality(0.8% vs 2.7%,P < 0.05)but a higher rate of intestinal obstruction(4.6% vs 2.2%,P = 0.001)was also observed when comparing CDI with NAFLD to ALD.CONCLUSION Hospitalized CDI patients with NAFLD had more intestinal complications compared to CDI patients with VLD and ALD.Gut microbiota dysbiosis may contribute to the pathogenesis of intestinal complications.
Key Words:Nonalcoholic fatty liver disease;Clostridioides difficile infection;Gut microbiota;Intestinal complications;Alcoholic liver disease;Viral liver disease
INTRODUCTION
Nonalcoholic fatty liver disease(NAFLD)is a heterogeneous disease with a spectrum from simple steatosis to nonalcoholic steatohepatitis(NASH),cirrhosis,and hepatocellular carcinoma[1,2].With a prevalence of 10 to 46 percent in the United States and 6% to 35% worldwide[3,4],NAFLD has become the leading cause of chronic liver disease,and its prevalence continues to increase,paralleled by the increase of obesity and type 2 diabetes[5].
Clostridioides difficile(C.difficile)is a gram-positive,spore-forming bacterium,known as the most common pathogen causing nosocomial diarrhea in developed countries[6].Symptoms ofC.difficileinfection(CDI)range from mild to severe diarrhea,which can progress to sepsis,fulminant colitis,and bowel perforation[7].Severe colitis may also present as ileus and megacolon,which are characterized by symptoms of intestinal obstruction[8,9].Gut microbiota dysbiosis due to the administration of antibiotics is the most prominent risk factor for the development of CDI.Advanced age,prolonged hospitalization and gastric acid suppression are some common additional risk factors for CDI[10,11].
Recently,a number of animal and human studies have revealed the role of the gut microbiota in the pathophysiology of NAFLD.It is proposed that dysbiosis-induced dysregulation of the gut barrier function and translocation of the bacteria link the gut microbiome to NAFLD[12,13].In addition,it has been well documented that patients with chronic liver disease are more susceptible to CDI due to frequent hospitalization and antibiotics use.Specifically,recent studies have observed that NAFLD is an independent risk factor for CDI by single-centered retrospective design[14,15].
Although a strong association between NAFLD and CDI has been observed,gut microbiota dysbiosis likely plays a vital role in the pathogenesis of both aforementioned diseases.However,the inpatient outcomes of CDI in the NAFLD population,have not been well studied in large populations.The aim of this nationwide study was to assess the impact of NAFLD on the outcomes of hospitalized patients with CDI.
MATERIALS AND METHODS
Data source and study population
The largest all-payer inpatient care database in the United States,the Nationwide Inpatient Sample(NIS)database was accessed.The NIS database represents approximately 20% of all inpatient hospitalizations.Weighted,it estimates more than 35 million hospitalizations nationally[16].It includes demographic information(age,sex,race,income),hospital characteristics(e.g.,bed size,type),insurance status,discharge status,diagnoses and procedures(identified by The International Classification of Diseases-Ninth Edition Revision Clinical Modification(ICD-9 CM)codes),total hospitalization charges,length of stay(LOS),severity and other comorbidity measures.Yearly sampling weights are applied to generate national estimates.
This retrospective cohort study examined all adult(18-90 years old)patients hospitalized with CDI as the primary diagnosis from 2010 to 2014.Within this CDI population,patients with NAFLD were selected to compare to those with viral liver disease(VLD)(including hepatitis B infection and hepatitis C infection)and those with alcoholic liver disease(ALD).Notably,CDI was identified by ICD-9 CM code 008.45.NAFLD was identified by ICD-9 CM code 571.80 with the exclusion of all diagnostic codes for previous organ recipients and donors as well as other causes of chronic liver disease including hepatitis B and hepatitis C infection,ALD,hemochromatosis,primary biliary cholangitis,autoimmune hepatitis,and other unspecified liver diseases.The diagnosis of VLD was identified by the ICD-9 CM codes for hepatitis B and C caused liver diseases with the exclusion of previous organ recipients and donors,as well as other causes of chronic liver disease including NAFLD,ALD,hemochromatosis,primary biliary cholangitis,autoimmune hepatitis,and other unspecified liver diseases.Similarly,ALD was identified by the ICD-9 CM codes for ALD with the exclusion of previous organ recipients and donors as well as other causes of chronic liver disease including NAFLD,VLD,hemochromatosis,primary biliary cholangitis,autoimmune hepatitis,and other unspecified liver diseases(see Supplementary Table 1,supplemental digital content 1,which demonstrates ICD-9 diagnostic and procedure codes).VLD and ALD were assessed as separate groups which excluded patients with concomitant diagnoses of VLD and ALD.Information such as patients’ demographics,comorbidities,disposition,selected outcomes and surgical interventions were extracted from the NIS database.Elixhauser Comorbidity Index(ECI)[17],which measures 29 general medical conditions,then assigns different weights to compile a longitudinal score,allowing for further description of comorbidity burden.
Primary outcomes included mortality,length of stay,and total hospitalization charges.Secondary outcomes were CDI related complications and interventions.
Statistical analysis
SAS Survey Procedures(SAS 9.4,SAS Institute Inc,Cary,NC,United States)was utilized for all statistical analyses.The national estimates were calculated after accounting for sample design elements(clusters,strata,and trend weights)provided by the NIS.Continuous variables were reported as weighted mean ± SE;categorical variables were reported as weighted numbers(n)and percentages(%).The SEs of weighted means were estimated using the Taylor linearization method that incorporated the sample design.Weighted Student’st-tests were used to analyze the normally distributed continuous variables,while Rao-Scott modified chi-square tests were used to test the difference of distribution for categorical variables.Wilcoxon Rank-Sum Tests were used to test the variables that are not normally distributed.Multivariate linear regression was used to estimate the average change in LOS and total hospitalization charges after adjusting for patient demographics,hospital characteristics,insurance type,median household income,ECI score,obesity,diabetes,tobacco use disorder,hypertension,dyslipidemia,cirrhosis and its complications,numbers of cirrhosis complications,and hepatocellular carcinoma.Multivariate logistic regression was used to estimate the odds ratio(OR)of mortality,CDI complications and interventions after adjusting for the same confounding variables as noted above.
The statistical methods of this study were reviewed by Dr.Chunyi Wu,PhD of Epidemiology from University of Michigan Medical School.
RESULTS
Patient demographics and baseline characteristics
From 2010 to 2014,the numbers of patients hospitalized for CDI with coexisting NAFLD,VLD and ALD were 7239,11857 and 5938,respectively.The CDI with NAFLD cohort in this study was predominantly Caucasian with an average age 56.3 years old.In the aforementioned cohort,69.4% of the patients were female,41.6% were admitted to southern hospitals,and 58.6% were admitted to large hospitals(Table 1).Compared to CDI with VLD or ALD individually,the CDI with NAFLD group had significantly more patients in the 18-39 and greater than 70-year-old age groups(P <0.0001),were more likely to be female(P <0.0001),from the southern hospital region(P <0.0001),and less likely to be Medicaid insured(P <0.0001).Additionally,the CDI with coexisting VLD group was associated with a higher percentage of African American patients and had less patients with a high household income(Q3 and Q4,median household income for ZIP code between 51th and 100th percentile)compared to the CDI with NAFLD group.
In regard to comorbidities(Table 2),when compared to the CDI with VLD or ALD groups individually,CDI patients with NAFLD had a greater prevalence of obesity(P <0.0001,P <0.0001),diabetes(P <0.0001,P <0.0001),hypertension(P= 0.0006,P <0.0001)and dyslipidemia(P <0.0001,P <0.0001).CDI with NAFLD was also associated with a significantly lower rate of cirrhosis(P <0.0001,P <0.0001)when compared to the other two groups.None of the patients in the CDI with NAFLD group had cirrhosis-related ascites,esophageal varices bleeding,spontaneous bacterial peritonitis or hepatorenal syndrome.Moreover,a lower rate of hepatocellular carcinoma(P <0.0001,P= 0.0217)was observed in the CDI with NAFLD group compared to the CDI with VLD or ALD groups individually.
Outcomes and regression analysis of CDI patients with NAFLD vs VLD
When compared to the CDI with NAFLD group,the CDI with VLD group was associated with higher rates of acute kidney injury(AKI)[adjusted OR(aOR)= 1.35,95%CI:1.10-1.67,P= 0.0041],respiratory failure(RF)(aOR = 1.83,95%CI:1.22-2.76,P= 0.0036),longer LOS(adjusted LOS ratio = 1.12,95%CI:1.06-1.18,P <0.0001)and higher hospitalization charges(adjusted cost ratio = 1.13,95%CI :1.06-1.2,P <0.0001).However,a lower rate of intestinal perforation rate was observed in the CDI with VLD group(aOR = 0.12,95%CI:0.03-0.57,P= 0.0075).CDI with VLD was initially associated with higher rates of mortality,colectomy and ileostomy,however this difference no longer existed after adjusting for confounding factors(Table 3).
Outcomes and regression analysis of CDI patients with NAFLD vs ALD
When compared to CDI patients with NAFLD,CDI patients with ALD had higher rates of RF(aOR = 1.72,95%CI:1.09-2.72,P= 0.0201),mortality(aOR = 2.63,95%CI:1.25-5.51,P= 0.0107),longer LOS(adjusted LOS ratio = 1.18,95%CI:1.10-1.25,P <0.0001)and higher hospitalization charges(adjusted cost ratio = 1.17,95%CI:1.09-1.26,P <0.0001).However,a lower rate of intestinal obstruction(aOR = 0.45,95%CI:0.28-0.72,P= 0.0010)was found in the CDI with ALD group when compared to the CDI with NAFLD group.Higher rates of AKI and septic shock,and a lower rate of colectomy were initially observed in CDI with ALD group,but the difference no longer existed after adjusting for the aforementioned confounders(Table 4).
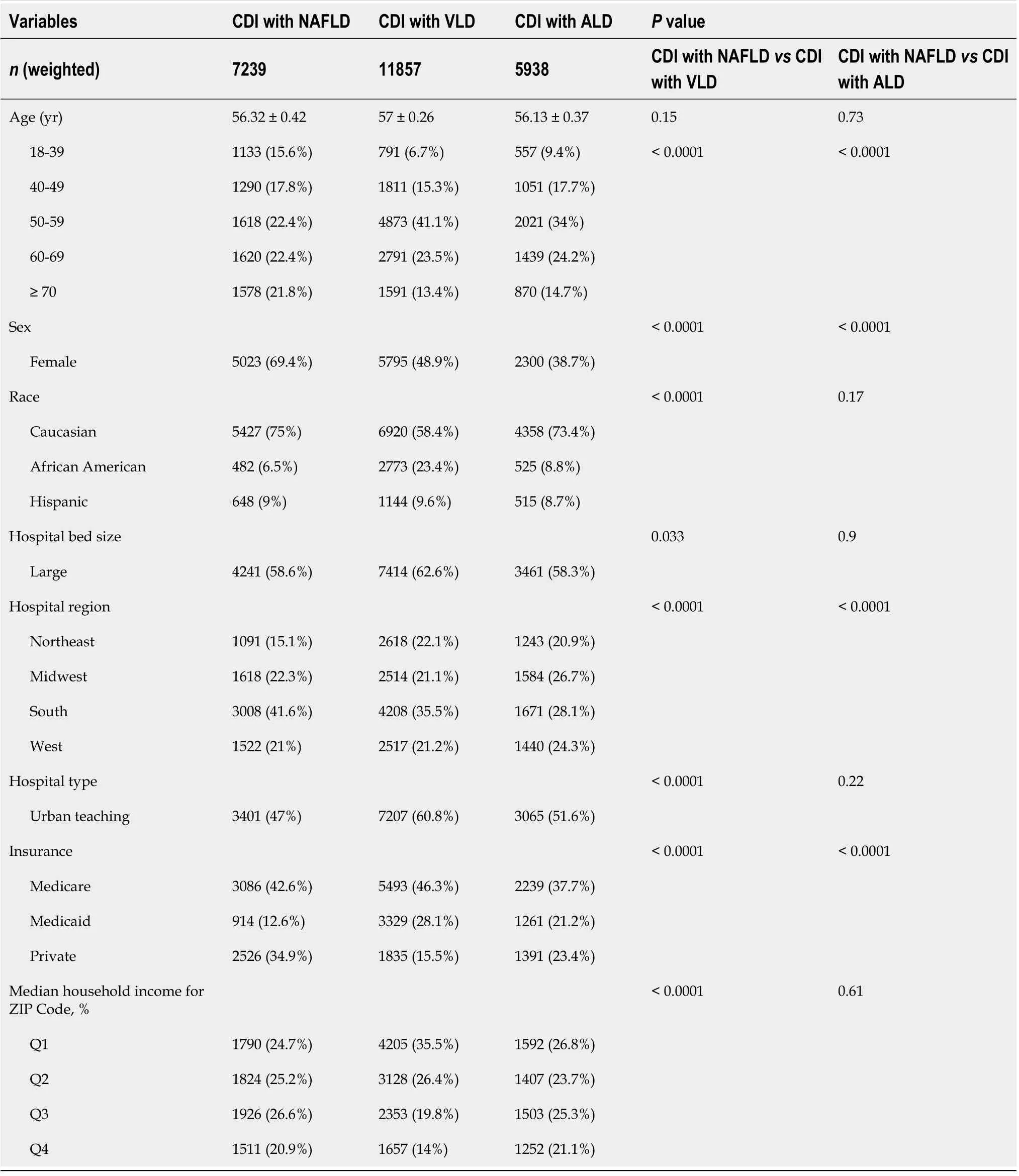
Table 1 Comparison of demographic data for patients hospitalized with Clostridioides difficile infection with coexisting nonalcoholic fatty liver disease,viral liver disease and alcoholic liver disease
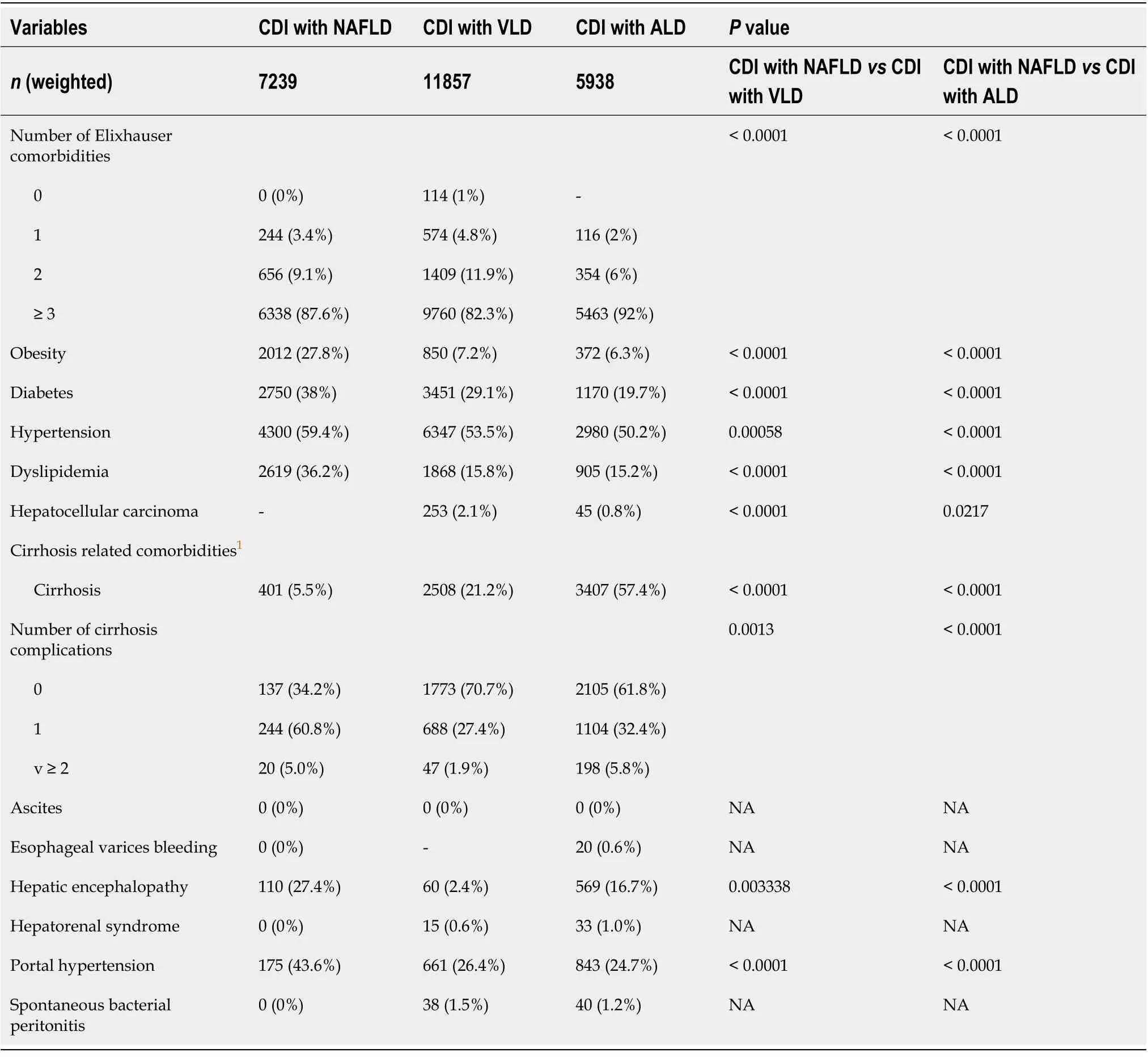
Table 2 Comparison of comorbid conditions and complications for patients hospitalized with Clostridioides difficile infection with coexisting nonalcoholic fatty liver disease,viral liver disease and alcoholic liver disease
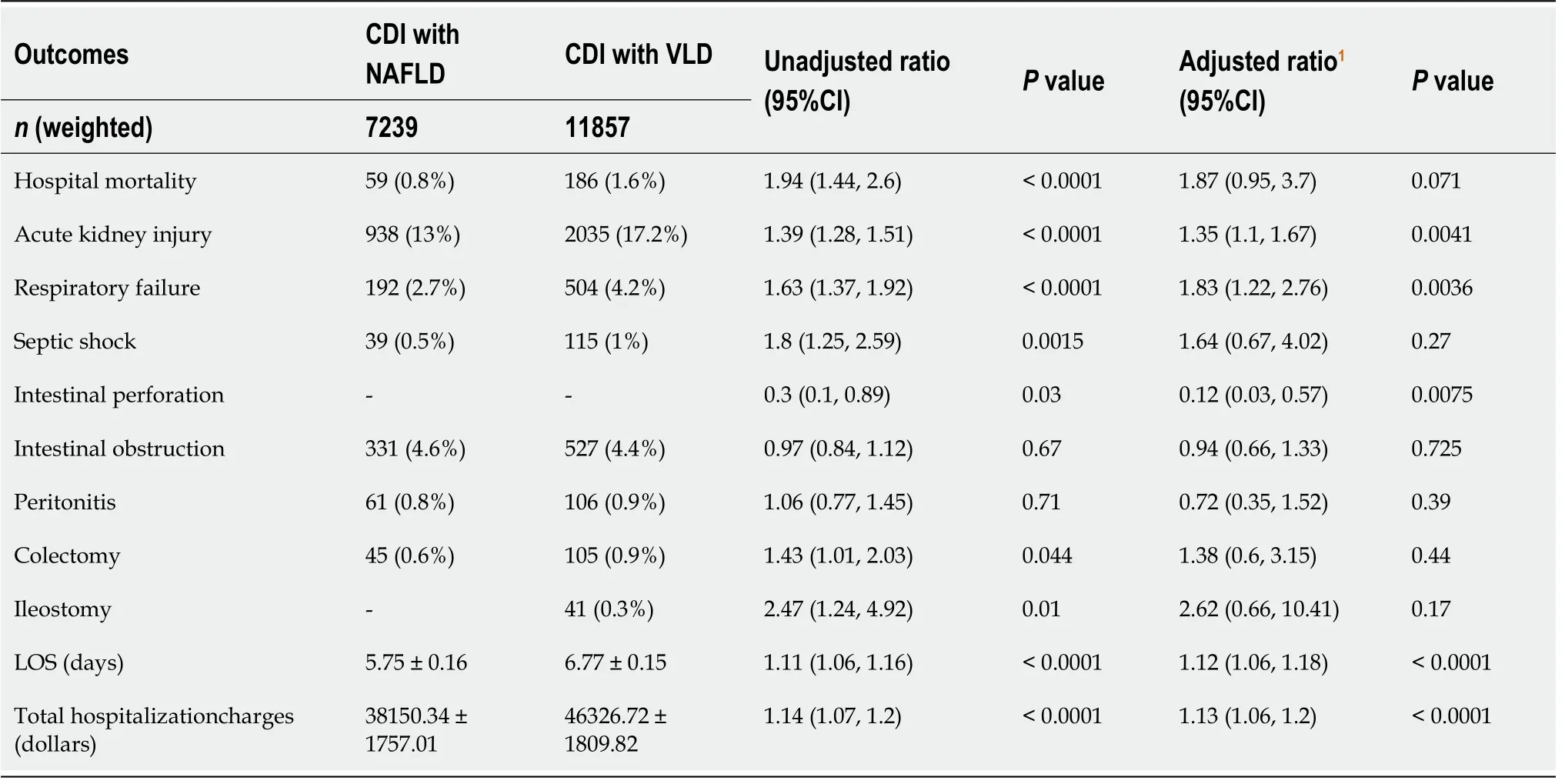
Table 3 Multivariate regression analysis of outcomes for patients hospitalized for Clostridioides difficile infection with coexisting nonalcoholic fatty liver disease vs viral liver disease
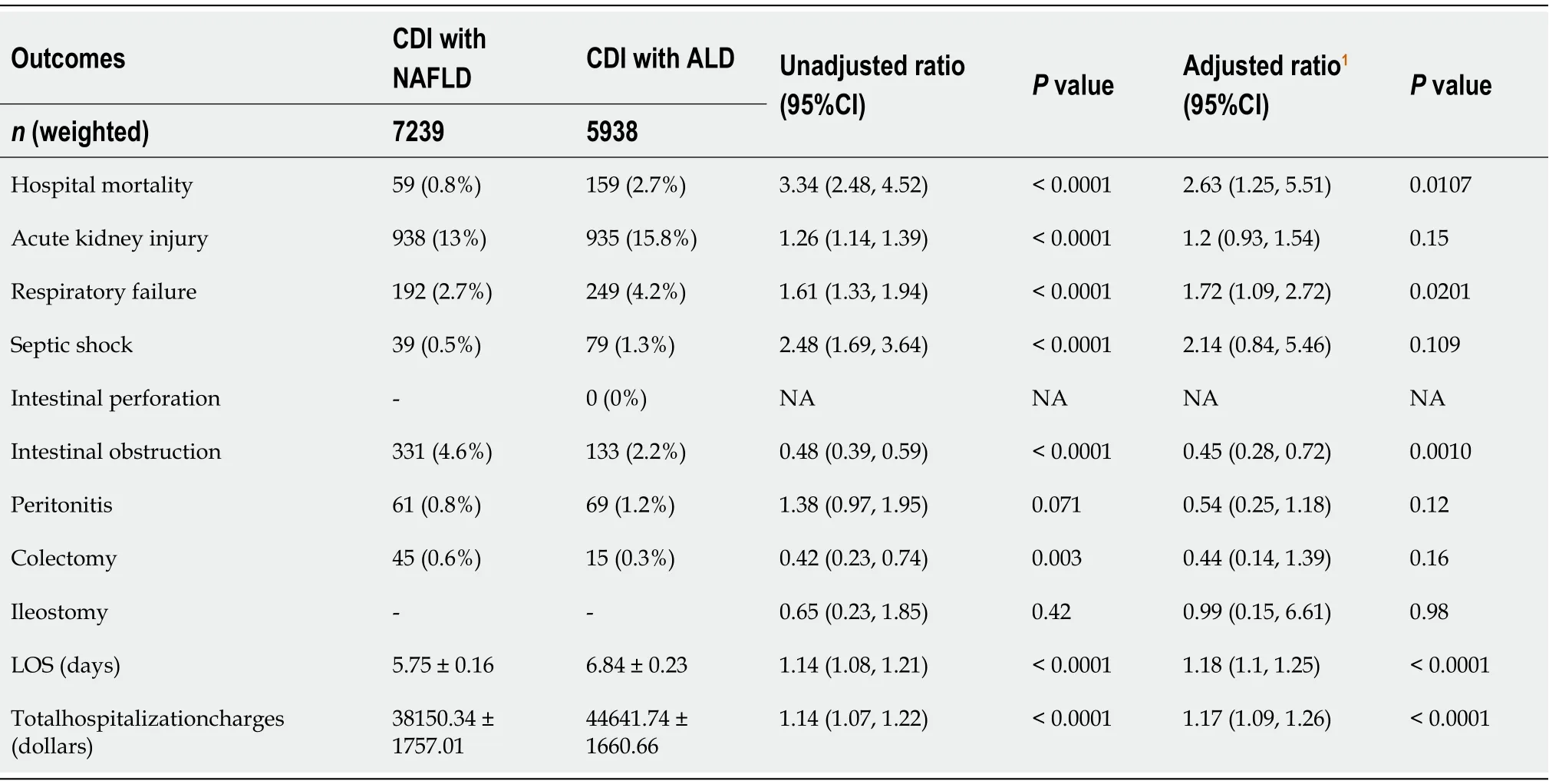
Table 4 Multivariate regression analysis of outcomes for patients hospitalized for Clostridioides difficile infection with coexisting nonalcoholic fatty liver disease vs alcoholic liver disease
DISCUSSION
This nationwide retrospective cohort study investigated the inpatient clinical characteristics and outcomes of CDI in hospitalized patients with coexisting liver diseases,with comparisons between NAFLD,VLD and ALD.We demonstrated that patients hospitalized with CDI and coexisting NAFLD had overall more favorable outcomes including a lower rate of RF,lower hospitalization charges and a shorter LOS whencompared to those with ALD and VLD individually.Interestingly,higher rates of intestinal complications were observed in the CDI with NAFLD group when compared to the CDI with ALD or VLD groups.Specifically,a significantly higher rate of intestinal obstruction was seen in the CDI with NAFLD group when compared to the CDI with ALD group,and a higher rate of intestinal perforation was seen when compared to CDI patients with concomitant VLD.
Our findings of worse intestinal complications in patients hospitalized with CDI and coexisting NAFLD compared to CDI patients with VLD and ALD,linked the gut pathology to the liver.The crosstalk between the gut and liver is increasingly recognized as the gut-liver axis[18].Receiving more than 70% of the blood supply from the intestinal venous outflow,the liver represents the first line of defense against gut derived antigens with a broad array of immune cells[19].The liver also releases many bioactive mediators into the systemic circulation,allowing for communication with the intestine.In the intestine,the endogenous and exogenous products from host and microbial metabolism translocate to the liver through the portal venous system,ultimately influencing liver function[20].
How does NAFLD influence the intestinal complications of CDI through the gutliver axis? Convincing evidence has shown that NAFLD is associated with significantly increased gut permeability and inflammation in both animal[21]and human models.Mieleet al[22]found that NAFLD patients had significantly increased gut permeability measured by urine radiolabeled markers and immunohistochemical analysis of zona occludens -1 expression in intestinal biopsy specimens,compared with healthy volunteers.They also discovered that both gut permeability and the prevalence of small intestinal bacterial overgrowth are correlated with the severity of steatosis.Verdamet al[23]found that plasma immunoglobulin G levels against endotoxin were increased in NASH patients,which positively correlated with the severity of inflammation.Furthermore,transmission electron microscopy observed irregular microvilli and widened tight junctions in the gut mucosa of the NAFLD patients[24].In addition,decreased numbers of CD4+ and CD8+ T lymphocytes and increased levels of TNF-α,IL-6 and IFN-γ were detected in the NAFLD patient group compared to healthy control.All of these results suggested impaired gut permeability and increased levels of inflammation at both the tissue and cellular levels in NAFLD disease models.
The gut microbiota-mediated inflammation,the related disturbance of the intestinal integrity and the impairment in mucosal immune function have been reported to play important roles,not only in the pathophysiology of CDI[25]but also in the pathogenesis of NAFLD[13,24,26].The gut microbiota normally exerts significant influence on intestinal epithelial cell health,nutrient metabolism and mucosal defense[19,27].Early evidence in animal studies demonstrated that altered gut microbiota composition[28]independently contributed to the development of NAFLD in mice.In addition,altered interaction between the gut and the host(produced by defective inflammasome sensing in inflammasome-deficient mouse models)may govern the rate of progression of multiple metabolic syndrome-associated abnormalities[29].With the recent developments in genome sequencing technologies,bioinformatics,and culturomics;it has been recognized that NAFLD and NASH are associated with decreased richness of the gut flora and increased risk of pathogenic flora in pediatric and adult patients[30-34],which are both well known risk factors for CDI.Although it is still unclear which specific microorganisms are harmful given conflicting results inhuman and animal studies[35],it is believed that gut microbiota-derived signatures extracted by whole-genome shotgun sequencing of DNA can be used for diagnosis of advanced fibrosis in NAFLD[36],and modification of gut microbiota analyzed by 16S ribosomal RNA pyrosequencing can be used for therapeutic purposes in NASH patients[37].Additionally,increased pathogenic flora in NAFLD and NASH further disturb the immune balance and cause worsened dysbiosis through various mechanisms involving short-chain fatty acids[38],lipopolysaccharide[21],choline metabolism[39],bile acid metabolism[40]and bacteria-derived ethanol[41].Collectively,NAFLD and NASH related alterations of gut microbiota and its downstream dysbiosis pathways may contribute to CDI risk and worse intestinal complications.
On the other end,we sought to identify the characteristics of gut microbiota changes in ALD and VLD.Compared to NAFLD,ALD is remarkably similar histologically[42]and initiated directly from the gut by alcohol intake or binges.It has been well documented that alcohol intake can lead to changes in gut microbiota composition[43]and gut permeability[44]early on,even before the development of liver disease.These alterations involve multiple physical and biochemical layers of defense in the intestinal barrier[19].In VLD,the gut microbiome works as an effective tool early on for immunity against the hepatitis virus,and helps with viral clearance[45].In chronic VLD,large translocations of intestinal microbiota were observed and thought to contribute to not only dysregulation of immune cells and dysfunction of the intestinal barrier,but also viral replication[27].Comparison analysis revealed that,compared to other cirrhosis etiologies,alcoholic cirrhosis is associated with worse gut dysbiosis after adjusting for Model For End-Stage Liver Disease score and body mass index[46].In two other studies[47,48],which primarily compared the gut microbiota composition in HBV/HCV related and alcoholic cirrhosis,no difference was observed at the phylum and class level.
Intriguingly,in our study,the majority(94.5%)of patients in CDI with NAFLD group were non-cirrhotic;the percentage of cirrhotic patients in CDI with NAFLD group was significantly less than those in CDI with ALD or VLD group.CDI with NAFLD group was associated with a higher rate of intestinal complications after adjusting for cirrhosis and its complications.These results suggested that NAFLD is associated with altered gut microbiota that is predisposed to CDI and its complications,likely independent from the liver disease severity.In fact,NAFLD has been reported as an independent risk factor for CDI[14].Although ALD and VLD cirrhosis was previously found to be associated with worse gut dysbiosis than NAFLD cirrhosis,this finding should be treated cautiously for non-cirrhotic patients,because the alteration of the gut microbiome is associated with the severity of liver disease,as significant differences in gut microbiota have been found between non-cirrhotic,compensated and decompensated cirrhotic patients[49,50].Importantly,the standard of care therapies in cirrhotic patients such as lactulose,rifaximin,antibiotics and acidsuppressants that can affect the gut microbiota,may be playing a critical role[51].In summary,our study suggested that NAFLD may be associated with worse dysbiosis in early liver disease stages and therefore a higher risk for CDI and its complications compared to ALD and VLD.
Aside from aforementioned gut microbiota changes that directly link NAFLD to CDI and intestinal complications,NAFLD related metabolic syndrome and systemic inflammation also play crucial roles in intestinal pathology.Recently,metabolic dysfunction-associated fatty liver disease has been proposed as a more appropriate name to replace NAFLD by an international panel of experts,with emphasis on the underlying metabolic dysfunction[52,53].Clinical evidence has demonstrated that NAFLD,along with other components of metabolic syndrome,such as diabetes and obesity,are associated with an increased prevalence of small intestinal bacterial overgrowth(SIBO)[54,55]by insulin resistance,oxidative stress and chronic low grade inflammation[56].Subsequently,the dysmotility induced by SIBO can further promote SIBO in NAFLD patients,causing a vicious cycle[57].In fact,dysmotility itself is associated with NAFLD and may be a potential therapeutic target for NAFLD from a Japanese study[58,59].Moreover,diabetes,a component of metabolic syndrome which may cause vasculopathies and neuropathies in the intestines,also contributes to dysmotility[60].Additionally,diverticular disease,irritable bowel disease[61]and inflammatory bowel disease[62],together with SIBO and dysmotility have all been shown to have increased prevalence in NAFLD patients.Not surprisingly,the structural and functional abnormalities in the gut associated with NAFLD and metabolic dysfunction further increase the risk of CDI and its complications.
The strengths of this study include the utilization of the NIS database to provide a unique opportunity to investigate a nationwide population hospitalized for CDI.To the best of our knowledge,this study is a leading clinical research analysis that provided a comprehensive nationwide comparison of outcomes between NAFLD and other common chronic liver diseases,ALD and VLD,in hospitalized CDI patients.There are also limitations in this study.Particularly,NIS data acquisition relies on the accuracy ICD-9-CM codes for medical diagnoses and no lab results,biopsy or image studies were available for NAFLD diagnosis and severity stratification.It is also difficult to determine which cases of CDI were hospital acquired or community acquired because ICD-9 codes are assigned at discharge.To strengthen the validity of ICD-9 codes for NAFLD,VLD and ALD,we used not only diagnostic codes but also excluded the codes for all other chronic liver diseases(Supplementary Table 1)[63].The ICD-9 codes for CDI were validated previously with good diagnostic accuracy[64,65].
CONCLUSION
In conclusion,this study found more favorable overall outcomes but higher rates of intestinal complications in patients hospitalized with CDI and coexisting NAFLD,compared to CDI with coexisting ALD and VLD,individually.These results suggested that NAFLD may be associated with a higher risk of CDI associated intestinal complications through alteration of gut microbiota.Our study also suggested that NAFLD associated metabolic syndrome may contribute significantly to the gut dysbiosis even in the early liver disease stages and cause increased risk for CDI and its complications.During the last few years,the novel and rapidly evolving research technologies for the gut microbiome have been opening up an exciting era in the microbiota therapeutics for different disease models[66].Tremendous progress has been observed in the treatment of NAFLD and CDI through gut microbiome manipulation.Our study may help increase awareness and diagnose intestinal complications in patients with two common diseases:CDI and NAFLD.Unraveling the significance of interactions between gut microbiota,gut immunity and systemic metabolic impact of NAFLD with prospective studies will provide more insights into the future microbiota therapeutics for CDI and NAFLD.
ARTICLE HIGHLIGHTS
Research background
The ongoing exploration of liver-gut axis has discovered strong association between gut dysbiosis and nonalcoholic fatty liver disease(NAFLD)in both basic science and clinical research.Small-scaled studies have observed that NAFLD is an independent risk factor forClostridioides difficileinfection(CDI).
Research motivation
CDI,as the most common cause of nosocomial diarrhea in developed countries,carries high hospitalization burden.NAFLD,as the leading cause of chronic liver disease,is commonly seen in hospitalized patients with CDI.So far the inpatient outcomes of CDI in the NAFLD population have not been well studied.
Research objectives
The authors aimed to examine the impact of NAFLD on the inpatient outcomes of hospitalized patients with CDI,by comparing the effect of NAFLD with alcoholic liver disease(ALD)and viral liver disease(VLD)individually.
Research methods
This nationwide retrospective cohort study was conducted according to STROBE statement using the National Inpatient Sample database.Inpatient CDI with coexisting NAFLD cases were selected using ICD-9 codes.Multivariate regression analysis was used with adjustment for a large group of possible confounders.Elixhauser Comorbidity Index(ECI)was used for a full description of comorbidity burden.
Research results
CDI with NAFLD was independently associated with lower rates of acute respiratory failure,shorter length of stay and lower hospitalization charges when compared to CDI with VLD and CDI with ALD.However,CDI with NAFLD was associated with a higher rate of intestinal perforation when compared to VLD,and a higher rate of intestinal obstruction when compared to ALD.
Research conclusions
CDI and coexisting NAFLD is associated with favorable overall outcomes,but higher rates of intestinal complications compared to CDI with coexisting ALD and VLD,individually.
Research perspectives
This finding suggests that alteration of gut microbiota may play an important role in the pathogenesis of both CDI and NAFLD.NAFLD associated metabolic syndrome may contribute significantly to the gut dysbiosis and cause increased risk for CDI and its complications.This study provides potential directions for future prospective clinical research to identify the clinical meaningfulness of interactions between gut microbiota,gut immunity and systemic inflammation.The study may open the door for potential microbiota therapeutic targets and manipulation as future treatment options for chronic liver diseases.
ACKNOWLEDGEMENTS
The authors thank Dr.Chunyi Wu,PhD of Epidemiology from University of Michigan Medical School for her assistance with the statistical analysis.
 World Journal of Hepatology2021年11期
World Journal of Hepatology2021年11期
- World Journal of Hepatology的其它文章
- Incidence of umbilical vein catheter-associated thrombosis of the portal system:A systematic review and meta-analysis
- Six-minute walking test performance is associated with survival in cirrhotic patients
- Circulating microRNA 9-3p and serum endocan as potential biomarkers for hepatitis C virus-related hepatocellular carcinoma
- Tumor characteristics of hepatocellular carcinoma after direct-acting antiviral treatment for hepatitis C:Comparative analysis with antiviral therapy-naive patients
- Cystic fibrosis associated liver disease in children
- Mitochondrial hepatopathy:Respiratory chain disorders- ‘breathing in and out of the liver’
