Circulating tumor cells and the metastatic process:the complexity of malignancy
Tania Di Raimo, EIena De Santis, Luigi CoppoIa, Mario Rosario D'Andrea, Francesco AngeIini
1Medical Oncology and Anatomic Pathology Unit, San Filippo Neri Hospital, Rome 00135, Italy.
2Experimental & Clinical Pharmacology, Centro Di Riferimento Oncologico - National Cancer Center, Aviano (PN) 33081, Italy.
3Department of Anatomical, Histological, Legal Medical and of the Locomotor Apparatus Sciences, Sapienza University, Rome 00135, Italy.
4Anatomic Pathology Unit, Sandro Pertini Hospital, Rome 00157, Italy.
Abstract Despite improvements achieved in terms of early detection and therapeutic approach, metastatic breast cancer remains one of the principal worldwide causes of death. In recent years, due to the heterogeneous response of each patient to chemotherapy, clinical research highlights the need of a personalized approach. Circulating tumor cells (CTCs) represents a promising tool for this purpose. Unfortunately, even if their correlation with severity, outcome and metastatic nature of the tumor has been established, several issues, mainly concerning their characterization and isolation, need to be solved. In this review, latest knowledge on CTCs and metastatic process in breast cancer were analyzed, aiming to understand their clinical utility and validity for a prospective therapeutic scenario.
Keywords: Breast cancer, metastasis, circulating tumor cells, personalized therapy
INTRODUCTION
Breast cancer (BC) represents the second leading cause of death among women not only in Western countries but also, as proved by new evidences, in developing countries[1-5]. BC has been de fi ned as a heterogeneous disease with multiple intrinsic tumor subtypes and the possibility to develop one of them is directly related to many factors, such as aging, genetics and lifestyle (obesity, lack of physical activity, sedentary behavior and frequent alcohol consumption)[6-8]. Furthermore, each BC subtype, with distinctive histopath-ological and biological characteristics, re fl ects different clinical outcomes and therapeutic strategies[6,9]. Estrogen and progesterone receptors (ER and PR) in addition to the human epidermal growth factor receptor 2 (HER-2) and the proliferation index (Ki-67) represent the most clinically used predictive biological markers[10,11]. Nowadays, it has been amply demonstrated how their expression is correlated with both BC intrinsic subtypes classi fi cation and the relative prognosis[6,12]. Concisely, the canonical molecular classi fi cation,fi rstly established by Perou in 2000, divided breast cancers in two principal subfamilies, ER- positive and ER-negative[6,12,13]. In the fi rst subfamily are included the LUMINAL A (ER+PR+HER2-Ki67-) and LUMINAL B (ER+PR+/-Her2+/-Ki67+) subgroups that represent the most common subtypes among BC. Despite the highest incidence, luminal A has the best survival rate and is recurrence-free, while luminal B, due to their heterogeneity, presents a worse outcome together with an high risk of relapse, thus additional chemotherapy and anti-HER2 drugs treatment are needed[14,15]. The ER- subfamily includes two principal subgroups. The fi rst subtype, called HER2 OVER-EXPRESSED (ER-PR-Her2+Ki67+), is correlated with poor prognosis and a higher risk of early relapse. Hopefully, it has been demonstrated that anti-HER2 drugs treatment brings an increment on survival and patients respond positively to chemo and neoadjuvant therapy[6]. The second ER- subgroup, the so-called BASAL LIKE, that represents 15% of BC, is characterized by an expression patterns including lack or low expression of ER, PR and HER2 in addition to a high expression of basal markers and Ki67. In the 60%-90% of cases, basal-like BC is TRIPLE NEGATIVE BC (TNBC), due to the absence of the principal three biological marker expressions[16]. TNBC represents a very heterogeneous subgroup comprised of further six subclasses, such as basal-like BL1 and BL2, mesenchymal-like, mesenchymal stem-like, luminal-androgen receptor expression, immunomodulatory and an unstable type subclasses[17]. In general, the TNBC subgroup exhibits, in addition to a high proliferation rate, an increase in basal/myoepithelial cells-related cytokeratins (CKs) and epidermal growth factor receptor (EGFR) expression[14].Furthermore, even if its heterogeneity is correlated with different prognosis and severity levels, the high percentage of TNBC patients present the worse clinical outcome, a shorter relapse-free period and a strong possibility to develop bone, lung, brain and liver metastasis[18,19]. Actually, it is clearly demonstrated that there is a strict correlation between the survival of women with BC and the incidence of distant metastases[20,21]. The migration of tumor cells from the primary tumor into the blood stream and their subsequent dissemination to secondary locations throughout the body represents thesinequanoncondition that acts as a trigger for the entire metastatic process[22]. Nowadays, circulating tumor cells (CTCs) represent an important prognostic biomarker in early BC disease and their presence is directly correlated with the patient's response to therapy and with poor prognosis in case of recurrence in radically resected BC or in metastatic disease[23-26]. Nevertheless, determination and utility of CTCs, in the common clinical practice, are still object of discussion[27]. Therefore, after a little excursion on CTCs characteristics and behavior during the metastatic process, the aim of this review is to make a point on clinical utility and validity of CTCs for a prospective therapeutic scenario.
CTCs AND THEIR PLASTICITY IN THE METASTATIC PROCESS
It is estimated that, at least in 90% of cases, metastases in distant organs represent an obstacle to the therapy and the primary cause of death in BC patients[23,28]. In the presence of metastatic cancers, chemotherapy is less effective on tumor cells and, as estimated by the American Cancer Society, only 22% of patients present a 5-year survival rate (www.cancer.org). Metastasis can be described as a complex dynamic multi-step process that begins with the intravasation of primary tumor-derived cells into blood or lymphatic vessels and goes on with the arrest, adhesion and extravasation of CTCs bringing to the colonization of distant organs[22,29,30]. Whenever these cells penetrate into the bone marrow, acquiring a status of dormancy, they are de fi ned as “Disseminated Tumor Cells” (DTCs)[31,32]. Since their fi rst detection in 1869 by Ashworth,several studies and clinical trials have demonstrated and con fi rmed, over the years, the strict correlation between detection and monitoring of CTCs in peripheral blood and metastatic BC (MBC), in terms of disease progression, prediction of treatment efficacy and overall-survival[33-43]. This concept has also been ratifi ed in the eighth edition of the AJCC Cancer Staging Manual, in which circulating CTCs and bone mar-row DTCs detection and enumeration have been included as important prognostic tools in both M0 and M1 BC classes[44]. The ability of CTCs to perform several functional and morphologic changes, conferring them a high degree of heterogeneity and plasticity, lie behind their clinical and therapeutic attractiveness.It has been deeply highlighted the important role of epithelial to mesenchymal transition (EMT) as an essential trans-differentiation process in many physio/pathologic mechanisms, such as mesoderm formation in embryonic development, tissue repair or fi brosis[45-47]. Generally, epithelial cells are de fi ned as adherent cells, expressing E-cadherin, a transmembrane glycoprotein involved in tight junctions' formation between adjacent cells, and CKs, such as CK8, CK18 and CK19, that exhibit an apicobasal polarity and a dense network of intercellular adhesion complexes that prevent them from migrating. In contrast, mesenchymal cells are single spindle-shaped cells that do not present intercellular junctions and, consequently, are able to migrate. In addition, mesenchymal cells generally exhibit a speci fi c proteins pro fi le such as vimentin, fibronectin and alpha-smooth muscle actin (α-SMA)[48]. Therefore, considering the fi rst part of the metastatic process, in which cells loss their epithelial nature, acquire a mesenchymal-like expression pro fi le and the detachment from the primary tumor site occurs, CTCs undergo EMT[49,50]. This multiple complex signaling system is triggered by the transforming growth factor-β (TGF-β) that enhanced cell migration, invasiveness and increased ability to counteract apoptosis[51]. In fact, it has been demonstrated that TGF-β is able to induce, in normal mammary epithelial cells, the phosphorylation of Smad2 and Smad3 and the activation of other EMT-related pathways, such as Notch, PI3K/AKT and Wnt[52,53]. This signal cascade activates EMT transcriptional factors, such as ZEB1, ZEB2, Twist, Snail and Slug, that downregulate the expression of E-cadherin[54-57]. Consequently, cell-cell adhesions are disintegrated, cytoskeleton fi bers and extracellular matrix (ECM) component undergo remodeling bringing a loss of cell basal-apical polarity and a strong motile and invasive properties acquisition[58,59]. Together with E-cadherin, another epithelial-speci fi c transmembrane protein, involved in EMT process, is the epithelial cell adhesion molecule (EpCAM). In normal conditions, this protein is localized in the intercellular space, where it is able to promote tight junctions formation and interact with E-cadherin, to maintain the epithelial integrity. On the contrary, in cancer tissue, after EMT-related cell-cell adhesion disintegration, EpCAM becomes ubiquitously distributed on the entire cancer cell surface and, for this reason, more easy to be detected with antibody-based assay. In view of this, CTCs have long been traditionally de fi ned positive for EpCAM and CK markers expression and negative for the hematopoietic marker CD45 (EpCAM+/CK+/CD45-). However, in 2014, Lustberget al.[60]identi fi ed different circulating cell populations in MBC patients composed of EpCAM-/CK+cells expressing mesenchymal markers, with few or no epithelial markers, and cells with both hematopoietic and epithelial markers pro fi le. This heterogenic nature of CTCs was also con fi rmed through several gene expression profiling. In fact, whilst they supported the correlation between CTCs, metastatic process and patient's overall-survival, to date no consensus has been established regarding biological markers to be used to identify these cells[61-63]. Currently, putting together different studies, among all the analyzed genes related to cell survival (IGFR1, FOXO3), the EMT process (TWIST1, SNAIL, SLUG, VIM) or tumor progression and invasion (HER2, CXCR4, uPAR, VEGFA, VEGFR, Cathepsin D) only CK19, mucin 1 (MUC1) and EpCAM result as the most accepted genes[61,64-68]. In addition, it has been demonstrated that metastasis exhibit, as primary tumors, an epithelial phenotype instead of a mesenchymal one, and that, using mice models,mammary tumors can promote an apparent EMT-independent lung metastatic process[69,70]. Considering all these evidences, an epithelial-mesenchymal plasticity (EMP) model has been proposed as a hallmark of CTCs in the metastatic process, in which circulating cells, during their migration to distant organs, are able to switch between a hybrid phenotype along the epithelial to mesenchymal spectrum conferring them the ability to adapt in different microenvironments[71-73].
CTCs migration modeIs

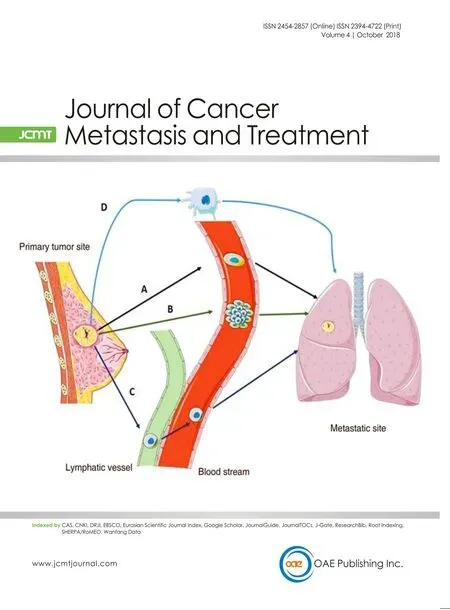
Figure 1. Cancer cells migration models. A schematic panel of tumor cells migration models discussed in the text: A: epithelial to mesenchymal transition/mesenchymal-epithelial transition process; B: collective migration model; C: lymphatic vessel pathway; D:mesenchymal to amoeboid transition process [Image created with Servier Medical Art (https://smart.servier.com/)]
In support of the EMP model, several histopathological, intravital microscopy andin vitrostudies demonstrated that CTCs exhibit different invasion strategies (collective or individual) and are able to exchange toward them according to the surrounding microenvironment[74-81][Figure 1]. The classical migration model depends on a reversible EMT process, known as mesenchymal to epithelial transition (MET). Primary tumor-derived CTCs, with a mesenchymal expression pro fi le and an elongated cell shape that allows them to adhere on ECM substrate and direct their migration, are able to penetrate in the blood stream[82]. Once reached a desirable metastatic niche, CTCs promote disruption of cell adhesion and polarity, remodeling of the cytoskeleton and changes in cell-ECM adhesion[83,84]. This tissue remodeling process leads to the generation of crossing points relevant for migration and tissue invasion[77]. Subsequently, mesenchymal CTCs are able to promote MET in order to restore their epithelial pro fi le as well as their proliferative ability. As a result, secondary tumor growth[78]is promoted. Instead of moving through the complex EMT/MET process,another proposed mechanism suggests that epithelial and mesenchymal cells could cooperate to migrate and promote the subsequent metastatic process. In the so-called “collective migration model”, it is assumed that hybrid phenotypes create and coexist in a multicellular cluster, called tumor micro-emboli or CTC cluster[85]. By comparing both collective and individual invasion mechanisms, it is clear that the cluster migration, instead of the individual one, provides several advantages to the metastatic process[77,82]. Functionally, this structure is able to guide migration and to invade the secondary organ thanks to the mesenchymal “l(fā)eader cells” that create a protective microenvironment to the poorly mobile but highly proliferate epithelial “follower” cells, inserted in the core, to accomplish the metastatic process[76,78,86]. A third mechanism, called mesenchymal to amoeboid transition, refers to a single dissociated primary tumor-derived cell that lost its attachment to the ECM adopting a distinctive spherical and highly deformable morphology with bubble-like protrusions, able to in fi ltrate tissues[77,87,88]. In contrast with the previous models, amoeboid migration, because it is a protease-independent process in which cells mechanically displace ECM fibrils instead of degrading them, represents at the same time a simple and efficient strategy to move through tissues and between tissue barriers[89,90]. The Met receptor tyrosine kinase (Met-RTK), a growth factor receptor, is able to promote tumor growth and metastasis by enhancing motility, survival, proliferation of cancer cells and stimulating angiogenesis[91]. In 2014, Laser-Azoguiet al.[87]demonstrated that BC cells ex-press high levels of activated Met-RTK which are able to induce membrane blebbing and, as a consequence,cell dissociation, amoeboid motility and invasion. Furthermore, they highlighted a Met-induced protection from apoptosis and the ability of these Met-expressing cancer cells to promote the metastatic process. The lymphatic vessel pathway, due to its discontinuous structure, the high concentration of hyaluronic acid and the lymph fl uid composition, which is able to improve cell survival and to reduced shear stress, represents a better and safer dissemination vehicle for cancer cells than the blood stream. Thus, it could be reasonable to consider the possibility that both epithelial and mesenchymal cancer cells migrate, preferably, through the lymphatic system, spread fi rst to lymph nodes and then drain into the blood[92-94]. Accordingly, another mechanism of tumor EMT-independent metastasis, namely tumor-induced lymphangiogenesis, has been proposed[95]. Briefly, mesenchymal cancer cells, which are able to produce and release lymphangiogenic factors, such as vascular endothelial growth factor C and D (VEGF-C and VEGF-D), promote an increase of lymphatic vessel density in the peri- and intratumoral area, so that epithelial cells are able to colonize lymphatic system and lymph nodes can facilitate their entry into the systemic circulation[96-100]. It has been demonstrated that an increase in lymph vessel density, due to tumor-induced lymphangiogenesis, is correlated with a high amount of lymph node metastasis, VEGF-C expression and worse disease-free/overall survival in BC patients[101].
Immune escape
An important issue related to the EMP of CTCs and their metastatic potential is the immune-escape, which is the ability of tumor cells, during their migration, to counteract the elimination by the immune system and to increase their possibility to survive and to colonize distant organs[102-104]. One of the most studied immune evasion mechanism is the programmed death-ligand 1 (PD-L1)/programmed death receptor (PD-1) axis. In normal conditions, the PD-L1 and its PD-1 represent a physiological checkpoint of the immune system.Antigen-presenting cells express PD-L1 while PD-1 is detectable on the surface of activated T-cells. Once ligand/receptor interaction occurred, a strong inhibitory signal promotes apoptosis and functional exhaustion in T-cells[105]. In 2014, Chenet al.[106]have identi fi ed, in lung tumor, a molecular link between the overexpression of the EMT-effector ZEB1 and a more abundant presence of PDL1, able to promote the exhaustion of intratumoral T lymphocytes and the development of metastasis[106-108]. Similarly, in breast cancer, it has been demonstrated that PD-L1 expression is heterogeneous and it is generally associated with the presence of poor-prognosis factors, high proliferative index and aggressive molecular subtypes[109,110]. In 2015, for the fi rst time, Mazelet al.[111]provided evidence that CTCs, isolated from the blood of BC patients,frequently express PD-L1 on their surface. The Fas/FasL axis represents another EMP-dependent immune escape mechanism based on the ligand/receptor interaction with a negative impact on the clinical outcome of BC patients[112]. Brie fl y, when the factor-associated suicide (Fas), a transmembrane receptor belonging to the tumor necrosis factor (TNF) family, interacts with its ligand (FasL), expressed on the surface of activated T lymphocytes, Fas-expressing cells go through apoptosis. During BC progression, Fas was found to be repressed in association with an increase of FasL level and TGF-β secretion in tumor cells, conferring to CTCs the ability to induce cell death and escape immune recognition[113].
Metastatic niche
Despite the migration mechanism and the above-mentioned immune evasion systems adopted by cancer cells, only a few percentage of cells that extravasate are able to survive in the unsuitable secondary organ environment and promote metastatic growth. Thus, the microenvironment in the metastatic site represents a major challenge for invading cancer cells. Starting from the “seed and soil” hypothesis, postulated by Paget, up to date, it is well known that cancer cells (the seed) require a speci fi c and compatible “soil”microenvironment, the pre-metastatic niche, which is able to evolve and to promote both cell engraftment,creating the metastatic niche, and cell proliferation, leading to the micro- to macro- metastatic transition[114-119]. Many evidences demonstrate how primary tumor site is able to modify, before cancer cells'arrival, the secondary organ microenvironment, stimulating the creation of the pre-metastatic niche[120].
Tumor-secreted factors, such as VEGF-A, TNF-α and TGF-β, are able to promote bone marrow-derived hematopoietic progenitor cells (BMDCs) recruitment in the secondary organ. Accordingly, BMDCs recruitment results in an ECM remodeling, upregulating fi bronectin (FN) and other molecules, such as MMPs,and stimulate angiogenesis[121]. Hypoxia-inducible factor (HIF) represents a major effector and adaptor in BC cells that, due to a massive and unregulated proliferation in association with vasculature dysfunctions, are exposed to a hypoxic microenvironment[122-124]. Lysil oxidase (LOX), one of the principal HIF-dependent BC secreted factor, is strictly correlated with tumor invasiveness and lung and bone metastasis formation. In the pre-metastatic organ, LOX is able to co-localize with fi bronectin and to modulate cell-ECM interactions[125]. Furthermore, through the interaction with type IV collagen, LOX recruits BMDCs and, in a second attempt, promotes the colonization of metastatic tumor cells[126-128]. In the matrix remodeling scenario, it has been demonstrated that the secretion of lysil oxidase-like 2 (LOX-2) is also able to induce αSMA expression in pre-metastatic fi broblasts, inducing their activation and the secretion of FN and LOX,generating a fi brotic microenvironment capable of supporting tumor cell persistence and survival[129,130].Finally, the primary cancer secretion of VEGF, TGF-β and TNF-α stimulates Angiopoietin-2 expression in the pre-metastatic niche increasing vascular permeability and, consequently, promoting the extravasation of CTCs so that metastatic process can move forward[131-133].
STATE OF THE ART IN CTCs ANALYSES
The intrinsic mark of rarity of CTCs, in addition to their highly heterogeneous nature, represents an obstacle to study their biology[134,135]. Nevertheless, several technologies are being developed for CTCs detection in patients' peripheral blood sample based on their knowing biological properties[136]. The most commonly used techniques are based on a combination of enrichment/isolation and detection procedures. In the fi rst phase, CTCs are separated from hematologic cells, especially leukocytes that, due to their similar physiochemical and biological properties, could contaminate tumor cell pool[134]. The enrichment procedures exploit physical (size, deformability, density and electrical charge) or biological characteristics (cell surface protein expression, viability and invasive capacity) of CTCs[137,138]. The detection step consists of immunostaining methods ranging from classic immunocytochemistry (ICC) or immuno fl uorescence to fl ow cytometry[138]. Furthermore, RT-PCR approach represents another option to detect tumor related mRNA transcripts in patients' blood. Although this method does not require a prior CTCs enrichment, the inability to provide CTCs enumeration deeply restricts its utilisation[138]. Regarding CTCs isolation from blood components, density gradient centrifugation, such as Ficoll-Hypaque, Percoll (GEHealthcare Life sciences),OncoQuick (Greiner Bio-One), Cytotrack, Accucyte-cyte fi nder, represents the most commonly physical properties-based technique[139-141]. Other exploited approaches are based on cell-size separation, such as micro fi ltration (Screen Cell, CellSieve, ISET, Parylene fi lter, Filtration/Sequential ICC) or micro fl uidic test that combines size and deformability properties of CTCs (Ephesia, HB-CTC-chip, Iso-Flux, OncoCEE,Parsortix system , the ClearCell FX or Vortex)[135,142-151]. Nevertheless, even if all the described isolation methods represent rapid and less expensive alternatives, they are generally hampered by blood cells-related false-positive results, thus making necessary the combination with other enrichment methods and the loss of large CTCs and CTC clusters due to the high heterogeneity of CTC size[136,152]. Immunological assays,based on the extremely speci fi c reaction between antibodies and the target antigens on the cell surface,provide a high purity rate of isolated CTCs[145,153-160]. Several of these techniques are based on EpCAM positive selection and, actually, the most standardized method is the CellSearch? system (Janssen Diagnostics),the only one approved by the U.S. Food and Drug Administration for CTCs enumeration in BC and other type of cancer[25,27,157,161]. Nevertheless, as reported by several clinical trials, in patients in which EMT occurring with the downregulation of EpCAM and other epithelial markers, this system may fail to capture the entire pool of CTCs and may result in false negative fi ndings[74,134,162-165]. Furthermore, it has been demonstrated that the lack of EpCAM+CTCs detection does not re fl ect a status of benign prognosis. In fact,it could be directly related with negative hormone receptors, high tumor grade, triple-negative disease,in fl ammatory BC and brain metastasis (OR = 6.17, 95%CI: 2.14-17.79;P= 0.001) or conversely with bone metastasis (OR = 0.47; 95%CI: 0.27-0.80;P= 0.01)[166]. Hence, it is important to understand, using different epithelial and/or mesenchymal markers, how de fi ned other clinically relevant sub-populations of CTCs.Accordingly, taking into account the attested probability of false-negative results, cell-surface vimentin and EGFR were suggested as alternative markers for detecting mesenchymal transitioned CTCs[136,167,168]. To recapitulate, the common issue underlined with positive selection procedures is to fail the capture of cells with low expression of EpCAM and non-epithelial phenotypes such as those that have undergone EMT.In addition, the isolated CTCs have reduced viability and this aspect represents an important obstacle to CTCs' biological characteristics understanding[137]. Otherwise, immunological methods based on negative selection are also available. The latters are commonly used to deplete cells that do not express CD45 leucocyte antigen or a cocktail of antibodies direct against red and white blood cells, such as RosetteSep, Easy-Sep, Dynabeads, mojoSort[137]. Cells isolated with this approach are relatively more viable but, at the same time, are highly impure. In fact, the puri fi ed cells pool contains epithelial and non-epithelial phenotypes together with normal blood vessel, stromal cells or other cells normally present in the circulation[137]. These evidences, as reported by a huge number of studies, con fi rm that the main challenge of CTCs isolation and characterization are the lack of speci fi c standardized procedures that strongly restrict their use in clinical practice[134,169,170].
CLINICAL RELEVANCE OF CTCS
Despite progress achieved in terms of prevention, diagnosis and treatment, drug resistance and tumor relapse, whose severity and probability are speci fi c for each patient, remain one of the principal issue in breast cancer. Therefore, as a good clinical practice, it has been established that a patient's 5-year follow up, since primary tumor, could lead to an early detection of recurrence or metastasis and to a more speci fi c and effi cient therapy[169]. Canonical tissue biopsy represent on one side a costly, painful and hard to repeat procedure. In addition, it is not able to provide a complete genetic or epigenetic tumor characterization in order to identify possible tumor phenotypical alteration[171]. In this optic, non-invasive liquid biopsies and the measurement of speci fi c blood-based biomarkers represent an effective alternative parameter to monitored invasive BC patients. Cancer Antigen 15-3 (CA 15-3), carcinoembryonic antigen, tissue polypeptide antigen,tissue polypeptide-specific antigen and the soluble form of HER2 represent the most detected serum BC biomarkers[172-174]. Nevertheless, even if it has been demonstrated a correlation between single or combined circulating biomarker levels and recurrence incidence, many issues need to be solved[175-178]. For instance,there are still problems associated with the lack of a validated clinically relevant level to establish, for each biomarker, a cut-off parameter[169]. Furthermore, it has been demonstrated that biomarker prognostic efficacy depends on the recurrence site. In fact, higher levels of biomarkers were detected in BC distant metastases,such as bone or liver, than in loco-regional or lung recurrence[179]. Additionally, these biomarkers are inappropriate to fi gure out mechanisms of therapy resistance[169]. For these reasons, nowadays, the detection of CTCs from patient blood samples appears as a powerful tool in the management of early and advanced BC patients[138]. CTC-based liquid biopsy represents a more informative tool, able to improve patients' selection and monitoring for target treatments, than conventional tumor tissue based- biomarkers that focused only on the primary tumor or metastases. Indeed, in the last few years, several studies highlighted the prognostic relevance of CTCs in MBC. In particular, it has been demonstrated that patients with a persistent CTCs count > 5 cell per 7.5 mL blood had a worse patient free survival (PFS) and overall survival (OS) compared to those that have CTCs < 5 at baseline and during follow-up[25,27,180-182]. Furthermore, due to their characteristics and minimally invasive procedures, the use of CTCs permits to evaluate the dynamic change of tumor over time for each patient that may impair the response to speci fi c targeted treatments[138,183]. From this point of view, CTC detection appears to hold promise of a better patients' management but up to date they are not still routinely used in clinical practice. In fact, CTC enumeration and variation during treatment were independent from any other baseline clinical or pathological characteristics and were not associated with pathological complete response[26,27]. Furthermore, as highlight by the SWOG S0500 randomize trial in advanced breast cancer, there is no evidence that changing or discontinuing therapy based on CTC level could improve patients' health outcomes, quality of life or cost effectiveness. In addition, PFS and OS showed no difference in outcome when patients were switched to an alternate regimen[180]. Thus, the American Society of Clinical Oncology guidelines affirm that the use of CTC count alone may be prognostic but not predictive for monitoring response to treatment for metastatic breast cancer[184]. Nevertheless, several clinical trials based on the comparison in HER2/ER/PR expression pro fi les between patient's biopsy, from primary tumor or metastatic site, and CTCs, demonstrated a discrepancy between biopsies and circulating cells that could have important therapeutic implications[185]. In fact, it has been revealed in HER2-and ER+BC patients the presence, respectively, of HER2+and ER-CTCs associated with an increased mortality risk, poor PFS and low OS[186-188]. Therefore, knowing that the switch between HER2-/+or ER+/-can occur after multiple courses in patients under HER2-targeted or ER-endocrine therapies, the monitoring of CTCs becomes crucial[189,190].Obviously, these evidences suggest a potential mechanism of a patient's speci fi c therapy-resistance, which is still unknown and under investigation in ongoing clinical trials[191]. In conclusion, despite several issues needing to be overcome, CTCs could be considered as a “real-time” liquid biopsy, able to provide important molecular information about patient's current disease and, hopefully, to suggest the suitable personalized treatment regimen[138].
CONCLUSION
At present, personalized medicine represents one of the principal aims of medical research. For this reason, even the improvement achieved in treatment options and the better clinical outcomes for BC patients,conventional tissue biopsies are considered, up to date, a poor diagnostic procedure. The growing interest in CTCs and their in progress validation as diagnostic and prognostic biomarker, could represent the tool for achieving this wishes of “personalization”. In fact, despite the still outstanding issues already covered in this review, CTCs could be crucial to the understanding of the complex BC heterogeneity, at the same time,they could be considered as a screening tool. Furthermore, their proved implication in the metastatic process and, most important, in chemoresistance, is stimulating the rapid development of new CTC isolation and single cell analysis platform. In the future, it is expected that the improvement in CTCs knowledge may pave the way to the discovery of new targets and to therapies that are more efficient.
DECLARATIONS
Authors' contributions
Conception and elaboration of the work: Di Raimo T, Angelini F
Provided administrative, technical, and material support: Di Raimo T, Angelini F
Revisiting the work critically for important intellectual content: Di Raimo T, D'Andrea MR, Angelini F
Final approval of the version: Di Raimo T, De Santis E, Coppola L, D'Andrea MR, Angelini F
AvaiIabiIity of data and materiaIs
Not applicable.
FinanciaI support and sponsorship
None.
ConfIicts of interest
All authors declared that there are no con fl icts of interest.
EthicaI approvaI and consent to participate
Not applicable.
Consent for pubIication
Not applicable.
Copyright
? The Author(s) 2018.