Nodal involvement and p16-staining in upper alveolar ridge and hard palate cancer
Edgar Salas, Pedro Sanchez, Juan Postigo, Carlos A. Castaneda, Miluska Castillo, Valeria Villegas,Luis Cano, Sandro Casavilca, Luis A. Bernabe, Carolina Belmar, Maria R. Villa-Robles, Raul Mantilla,Henry Guerra
1Head & Neck Surgery Department, Instituto Nacional de Enfermedades Neoplasicas, Lima 15038, Peru.
2Research Department, Instituto Nacional de Enfermedades Neoplasicas, Lima 15038, Peru.
3Faculty of Medicine, Universidad Peruana San Juan Bautista, Lima 15067, Peru.
4Pathology Department, Instituto Nacional de Enfermedades Neoplasicas, Lima 15038, Peru.
INTRODUCTION
Squamous cell carcinomas (SCC) of the hard palate and upper alveolus ridge are relatively rare[1].Prognostic factors and neck management in head and neck SCC (HNSCC) have been extensively studied in series of tongue or floor of mouth SCC, or on series with a mixture of SCC tumor sites[2]. Only small retrospective series have evaluated the behavior of hard palate and upper alveolus, and suggest that they have a low rate of regional node metastases[3-8]. However, recent studies find higher rates of both neck lymph node involvement and neck recurrence in these malignancies, and, there is a need to identify those aggressive cases that would benefit from more aggressive treatment[9,10].
Several clinicopathological features have been implicated in recurrence risk and prognosis in HNSCC.These include tumor size, nodal involvement, tobacco and alcohol consumption, and presence of human papillomavirus (HPV) infection[11,12].
The prevalence of HPV infection is higher in oropharyngeal squamous cell carcinoma (OPSCC) (35.6%)and has been associated with both better prognosis and higher response rate to chemoradiation[12,13].P16 staining is highly correlated with HPV infection in OPSCC and has also been associated with good prognosis[14-17]. There is no information about the rate of p16 expression in rare locations like hard palate and upper alveolar ridge.
The aim of the present study was to evaluate predictive factors associated with node involvement,prognostic factors, and prevalence of p16 staining in hard palate and upper alveolar ridge SCC.
METHODS
Study population
All patients treated at Department of Head and Neck at Instituto Nacional de Enfermedades Neoplasicas with maxillary SCC between January 1997 and December 2011 were screened for the study. Inclusion criteria included having a primary tumor located in the upper alveolar ridge or hard palate, having a squamous histology, and having history of resection of primary tumor. Patients with primary tumor of nasal cavity and paranasal sinuses were excluded. The procedure of neck management was selected by the Institute surgeon. It included neck dissection in cases of clinically involved lymph nodes and in cases of metastasis risk factors like greater depth of primary tumor deep invasion. Selection of ipsilateral or bilateral dissection was also determined by the Institute surgeon and took into account clinical factors like proximity to midline.
Information about clinicopathological variables was taken from patient files and pathology report. Data included age, gender, tobacco use, alcohol use, tumor subsite, depth of invasion, histologic grade, margin status, perineural invasion (PNI), lymphovascular invasion (LVI), clinical and pathological stage (TNM classification), surgical procedure, radiation or chemotherapy administration, and date of last follow-up or death. Some standard pathological features that were not reported in patient file were prospectively completed by a pathologist (LC). The institutional review board approval was obtained from The Instituto Nacional de Enfermedades Neoplasicas (Lima, Peru). Since the study was based on a secondary source and there was no contact with the patients, no informed consent was applied; however, the identity and personal data of patients’ medical records were protected at all times.
P16 immunohistochemistry assay
Pathologists evaluated H&E slides under light microscopy and the most representative tissue were selected. A 0.6-cm punch was taken from each formalin-fixed paraffin-embedded (FFPE) sample selected and was transferred to an empty paraffin recipient block in order to construct tissue microarrays (TMA).FFPEs samples were fixed for 6 to 8 h in 10% neutral buffered formalin and routinely processed with standard methodologies.
In total, 41 tissue cores were distributed into ten TMA blocks. Tissue sections were cut at 3 mm and floatmounted on adhesive (silanized) glass slides. Immunohistochemistry (IHC) for p16 status was performed using the DAKO EnVision? FLEX+ detection system together with the Autostainer Link instrument (DAKO Corp, Carpentaria, California) on FFPE tissue. Antigen was retrieved using EnVision? FLEX Target Retrieval Solution, High pH, and p16 was detected using p16 mouse monoclonal antibody (clone 16p04,JC2, BSB 5828, prediluted, Bio SB, Santa Barbara, California). The EnVision? FLEX+, Mouse, High pH, (LINK) Kit was used to perform the assay according to the manufacturer’s instructions. It contains the substrate chromogen 3-3′-diaminobenzidine (DAB), which, on staining, results in a brown-colored precipitate at the antigen site.
Positive p16 expression was defined as a strong and diffuse nuclear and cytoplasmic staining in at least 70% of the tumor cells.
Immunohistochemical evaluation was carried out by three pathologists in independent readings (LC, HG,and SC). Reports that varied among readers were reevaluated to determine a consensus.
Statistical analysis
The log-rank statistic was used for univariate analysis, and Cox proportional hazards regression was used for multivariable analysis. Categorical comparisons were carried out using the chi-square statistic or Fisher exact test. In all cases, the level of alpha was set at 0.05 a priori. Survival analysis was calculated using the Kaplan-Meier method. All analyses were performed in SPSS version 17.0 (SPSS, Chicago, IL).
RESULTS
Tumor primary location for this cohort was distributed in 5 patients for hard palate and 73 for upper alveolar ridge. Mean age was 64.47 years old and 55.1% were female. There were tabaquismo and alcoholism history in 10.3% and 6.4% cases, respectively. Two (40%) hard palate and 52 (71.2%) upper alveolar ridge tumors were clinically classified cT4, and 3 (60%) hard palate and 21 (28.8%) upper alveolar ridge tumors were clinically node-positive at presentation. Clinical stages I-IV of upper alveolar ridge SCC were found in 1 (1.4%), 13 (17.8%), 5 (6.8%) and 54 (74%) of cases, respectively. Clinical stages II-IV of hard palate SCC were found in 1, 1 and 3 cases, respectively [Table 1].
The primary tumor was resected in all cases (n= 78). Neck dissections were initially performed in 24 cases(21 in clinically node-positive and 3 in node-negative). Nineteen (79.16%) of cases who went to neck dissections had confirmed nodal metastases on pathological examination (including the 3 clinically nodenegative cases). Cervical metastases in these 19 node-positive cases were distributed between levels I(94.7%), II (73.7%), and III (26.3%). Extracapsular extension at presentation was noted in 7 specimens of upper alveolar ridge tumors.
In no instances were age (P= 0.329), location (P= 0.590), cT (P= 0.629), histological grade (P= 0.361),PNI (P= 0.825), or LVI (P= 0.080) associated with cervical metastases [Table 2].
Neck recurrences
Altogether, 18 patients (75%) developed cervical recurrences, and 8 (44.4%) of them went to neck dissection rescue (3 of them with additional radiation). Altogether, 18 patients (75%) developed cervicalrecurrences and 8 (44.4%) of them went to neck dissection rescue (3 of them with additional radiation).Ten patients did not go to surgery and treatment for them were: radiation alone (n= 2), radiation and chemotherapy (n= 2), chemotherapy alone (n= 2) or no-treatment (n= 4). Cervical metastases in these 18 cases of cervical recurrences were distributed between levels I (61.1%), II (100%) and III (27.8%).

Table 1: General features

Table 2: Relationship between clinicopathological features and lymph node involvement
Fourteen of the patients who were clinically node-negative (25.9%) and 4 of the patients who were pathologically confirmed node-positive at presentation (16.7%) had recurrences in the neck. The mean time to neck recurrence was 8.6 months (2 to 29 months). A factor associated with neck failure was high histological grade (P= 0.037). Recurrences were not associated with age (P= 0.725), cT (P= 0.754), N (P= 0.536), or PNI (P= 0.624) [Table 3].
Expression of p16
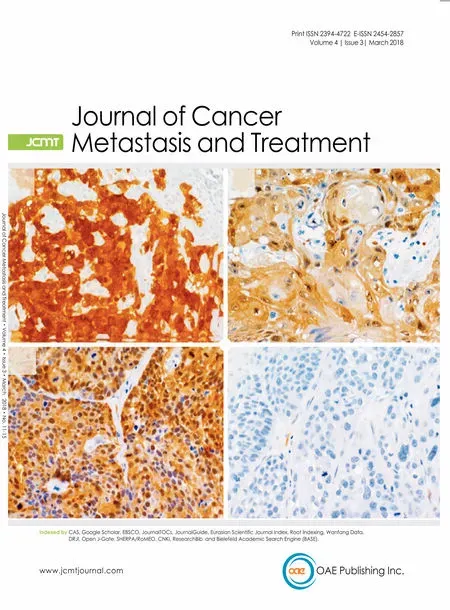
A total of 41 (52.5%) lesions were tested for p16 expression. Overall, 7.3% (3 of 41) were p16 positive: 1 of 2 in hard palate (50%) and 2 of 39 in alveolar ridge (5.1%) [Figure 1]. The p16 positive tumors were not associated with age (P= 0.067), tumor location (P= 0.143), cT (P= 1.000), or histological grade (P= 0.560)[Table 4].
Survival analysis
Median overall survival (OS) was 40 months. Neither smoking nor alcohol consumption was associated with shorter disease-free survival (DFS) (P= 0.815 and 0.507) nor OS (P= 0.597 and 0.634). LVI (P= 0.026)was associated with shorter DFS in univariate analysis. Larger cT (P= 0.019), presence of PNI (P= 0.039),LVI (P= 0.021), and neck dissection (P= 0.010) were associated with shorter OS in univariate analysis[Figure 2]. Neck involvement had a trend both for shorter DFS (31%vs. 48.7%,P= 0.278) and shorter OS(25.1%vs. 48.5%,P= 0.340). There was also a trend to shorter OS (9.3%vs. 52.3%,P= 0.064) in the presence of neck recurrence [Table 5].

Table 3: Relationship between clinicopathological features and neck recurrence (n = 78)

Figure 1: P16 by immunohistochemistry in upper maxilla. (A, B, C) Positive status of p16 staining indicated by brown staining of nuclear and cytoplasmic membrane in three cases; (D) negative status for p16 staining.(Magnification 40×)

Table 4: Relationship between p16 staining and clinicopathological features (n = 41)
DISCUSSION
Our rate of survival at 5 years was 44.5% and is similar to those reported by other studies (21% to 76%)[18,19].This poor prognosis could reflect higher prevalence of neck node involvement at diagnosis or higher prevalence of poor prognotic factors like p16-negative status[1].
The incidence of neck metastasis has been extensively described in cancer of the tongue and floor of the mouth (20% to 30%) and has been assigned a significant prognostic role in patients with clinically nodenegative disease[20,21]. Clinicopathologic factors like large tumor size, tumor depth, higher grade, and microvascular invasion have been associated with the development of cervical lymph node metastasis in oral SCC[21]. Elective treatment of the neck with staging neck dissection is generally carried out in patients with SCC of the oral cavity when the risk of clinically occult metastases exceeds 15% to 20%, and treatment of the clinically N0 neck is now accepted for certain oral cavity subsites, such as the tongue and floor of mouth, where elective neck dissection produces a survival advantage[22-26].

Figure 2: Estimated curves of OS regarding clinical tumor (A), perineural infiltration (B) and lymphovascular infiltration (C). OS: overall survival; PNI: perineural invasion; LVI: lymphovascular infiltration

Table 5: Survival analysis
The understanding of the behavior of hard palate and upper alveolar cancers is poor due to their low incidence and because some of these studies indistinctly included different both other head and neck malignancy locations and special pathological entities like salivary gland tumors[27,28]. A series of 606 upper and lower alveolar SCCs reported 37% of cervical metastasis and 19% of harbored occult disease in elective neck dissections. Lymph node involvement at level II to V carried shorter survival than negative lymph node involvement[19]. A series of 347 cancers of the upper and lower gums that had an elective neck dissection rate of 58% found occult disease in 5.6%. Neck recurrence was found in 9% of the whole group. Ipsilateral and contralateral neck node involvement predicted cervical recurrence. Positive neck lymph nodes, tumor stage, and involved soft-tissue margins were significant covariates in survival prediction; clinical stage remained significant in multivariate analysis[29]. A series of 252 cases of palate SCC including 62 in the specific region of the hard palate found node involvement in more than 29% of the hard palate tumors. Neck recurrence was predicted by the presence of fixed or contralateral node metastases, but not by the presence of nodal metastasis itself. Size of the primary tumor and histological grade was significantly associated with survival, and clinical stage was the most important prognostic indicator[30]. Recent retrospective series with 26 to 146 upper alveolar ridge and hard palate cases reported a neck lymph node involvement between 11% and 36.6%, and regional recurrence in N0 neck from 14% to 27%[1,5-8]. These studies had several findings: cases with neck node involvement had higher grade; clinical stage but not margin status was associated with prognosis; and T3 (55%) and T4 (52%) tumors exhibited higher rates of neck lymph node involvement than smaller tumors (T1 = 15%; T2 = 28%). An analysis of the Surveillance, Epidemiology, and End Results (SEER) database evaluated 314 hard palate SCC and 411 upper alveolar ridge cases. They found a 13.65% prevalence of cervical metastasis and its correlation with larger tumor (4.1% for T1 to 24.7% for T4 tumors,P< 0.001). Extension of lymph node involvement was correlated to survival (P< 0.001).
We found a neck lymph node involvement rate of 24.4% and it has a trend associated with shorter survival(P= 0.340). The traditional concept has been that SCC of the hard palate and maxillary alveolus exhibits a low rate of occult metastasis[7,31,32]. However, our results suggest that regional lymph node involvement is also frequent and relevant, and an elective treatment of the neck should be performed.
Regional recurrence rates in oral cancer have been described as between 30% and 47% in T1-2 carcinoma with untreated N0 neck, and they produce a significant decrease in patient survival. Some studies, including two prospective randomized trials, describe that neck recurrence rates decrease with the use of elective neck dissection[22,33-35]. Regional recurrences in oral malignancies were associated with poor differentiation, larger tumor size, positive lymph node, and extracapsular involvement[33,35]. A series of 114 cases with SCC of the maxillary alveolus and hard palate report regional recurrence rates of 26% in the N0 cohort (n= 100), and 35% of the patients had either initially N-positive neck or a later conversion from N0 to N-positive neck. Neck recurrence was associated with diminished overall survival but not with larger tumor size or postoperative radiation to the neck. Patients with initial diagnoses of N-positive and those who later developed neck recurrences had similar OS[36].
Neck node recurrences occurred in 18 cases (23.1%) of our series and appeared at a mean time of 8.6 months; this likely represents occult metastases at presentation. Therefore, we had 42.3% of neck node involvement if we consider initial patients with positive nodes and N0 patients who developed neck recurrence. We also found that 25.9% of cases without clinical evidence of neck involvement developed recurrences at the neck. Neck recurrence had a trend to poor prognosis but did not achieve significance,probably because these cases received effective treatment including surgery (44.4%) or chemoradiation(11.1%).
Large tumor size, PNI, and LVI have been extensively associated with nodal metastasis and with shorter survival in HNSCC[37,38]. Evaluation of classical prognostic factors in our series confirmed that larger tumors(P= 0.019), presence of PNI (P= 0.039), and LVI (P= 0.021) were associated with shorter OS, and LVI (P= 0.026) was associated with shorter DFS.
HNSCCs associated with smoking or drinking alcohol has been associated with a poor prognosis and are frequently located in laryngeal and hypopharyngeal cancer, respectively[39]. Our analysis did not indicate higher prevalence rates of these carcinogen agents and did not find an association with prognosis in the upper maxilla.
Expression of p16 is a confident biomarker of HPV infection in OPSCC and both are associated with better outcome[12,13,40-44]. In contrast to OPSCC, the rates of positive HPV in oral cancer are low, and recent studies suggest a disparity between the detection of HPV DNA and p16 expression when the prevalence of HPV is low[45]. Evaluation of p16 staining in our series found that only 3 (7.4%) of upper maxilla SCC cases were considered positive for p16 staining. The p16-positive cases had a trend to be younger (48.7vs.63.7 years,P= 0.067), and all 3 cases were free of neck recurrence and alive at 5 years. This is the first time to our knowledge that p16 staining has been evaluated in upper maxilla SCC and could identify a group of patients with specific behavior. However, our analysis has the weakness of its small sample size and it needs to be confirmed by larger series (required size of series increases because of the low rates of p16-positive status in non-OPSCC).
The results of this retrospective analysis reveal that tumors of the hard palate and upper alveolus are associated with a high rate of neck node involvement and regional failure, which had a tendency to result in poor survival. Expression of p16 has a low rate in this pathology and could be associated with specific features.
DECLARATIONS
The authors would like to express their gratitude to Vladimir Flores for their support in staining preparation of tumor sections.
Authors’ contributions
Conception and design of the study and performed data analysis and interpretation: Salas E, Castaneda CA, Sanchez P,Postigo J
Performed data acquisition, as well as providing administrative, technical, and material support: Castillo M, Villegas V, Postigo J,Cano L, Casavilca S, Bernabe LA, Villa-Robles MR, Mantilla R, Belmar C, Guerra H
Drafted the article and made critical revisions related to the intellectual content of the manuscript, and approved the final version of the article to be published: all authors
Data source and availability
No additional data are available.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
Patient consent
Not applicable.
Ethics approval
The institutional review board approval was obtained from The Instituto Nacional de Enfermedades Neoplasicas (Lima, Peru).
Copyright
? The Author(s) 2018.
1. Binahmed A, Nason RW, Hussain A, Abdoh AA, Sandor GK. Treatment outcomes in squamous cell carcinoma of the maxillary alveolus and palate: a population-based study.Oral Surg Oral Med Oral Pathol Oral Radiol Endod2008;105:750-4.
2. Balasubramanian D, Ebrahimi A, Gupta R, Gao K, Elliott M, Palme CE, Clark JR. Tumour thickness as a predictor of nodal metastases in oral cancer: comparison between tongue and floor of mouth subsites.Oral Oncol2014;50:1165-8.
3. Morris LG, Patel SG, Shah JP, Ganly I. High rates of regional failure in squamous cell carcinoma of the hard palate and maxillary alveolus.Head Neck2011;33:824-30.
4. Ogura I, Kurabayashi T, Sasaki T, Amagasa T, Okada N, Kaneda T. Maxillary bone invasion by gingival carcinoma as an indicator of cervical metastasis.Dentomaxillofac Radiol2003;32:291-4.
5. Simental AA Jr, Johnson JT, Myers EN. Cervical metastasis from squamous cell carcinoma of the maxillary alveolus and hard palate.Laryngoscope2006;116:1682-4.
6. Montes DM, Schmidt BL. Oral maxillary squamous cell carcinoma: management of the clinically negative neck.J Oral Maxillofac Surg2008;66:762-6.
7. Kruse AL, Gratz KW. Cervical metastases of squamous cell carcinoma of the maxilla: a retrospective study of 9 years.Head Neck Oncol2009;1:28.
8. Mourouzis C, Pratt C, Brennan PA. Squamous cell carcinoma of the maxillary gingiva, alveolus, and hard palate: is there a need for elective neck dissection?Br J Oral Maxillofac Surg2010;48:345-8.
9. Lin HW, Bhattacharyya N. Survival impact of nodal disease in hard palate and maxillary alveolus cancer.Laryngoscope2009;119:312-5.
10. Li Q, Wu D, Liu WW, Li H, Liao WG, Zhang XR, Liu ZM, Guo ZM, Liu XK. Survival impact of cervical metastasis in squamous cell carcinoma of hard palate.Oral Surg Oral Med Oral Pathol Oral Radiol2013;116:23-7.
11. Hashibe M, Brennan P, Benhamou S, Castellsague X, Chen C, Curado MP, Dal Maso L, Daudt AW, Fabianova E, Fernandez L, Wünsch-Filho V, Franceschi S, Hayes RB, Herrero R, Koifman S, La Vecchia C, Lazarus P, Levi F, Mates D, Matos E, Menezes A, Muscat J, Eluf-Neto J, Olshan AF, Rudnai P, Schwartz SM, Smith E, Sturgis EM, Szeszenia-Dabrowska N, Talamini R, Wei Q, Winn DM, Zaridze D,Zatonski W, Zhang ZF, Berthiller J, Boffetta P. Alcohol drinking in never users of tobacco, cigarette smoking in never drinkers, and the risk of head and neck cancer: pooled analysis in the International Head and Neck Cancer Epidemiology Consortium.J Natl Cancer Inst2007;99:777-89.
12. Ang KK, Harris J, Wheeler R, Weber R, Rosenthal DI, Nguyen-Tan PF, Westra WH, Chung CH, Jordan RC, Lu C, Kim H, Axelrod R,Silverman CC, Redmond KP, Gillison ML. Human papillomavirus and survival of patients with oropharyngeal cancer.N Engl J Med2010;363:24-35.
13. Fakhry C, Westra WH, Li S, Cmelak A, Ridge JA, Pinto H, Forastiere A, Gillison ML. Improved survival of patients with human papillomavirus-positive head and neck squamous cell carcinoma in a prospective clinical trial.J Natl Cancer Inst2008;100:261-9.
14. Namazie A, Alavi S, Olopade OI, Pauletti G, Aghamohammadi N, Aghamohammadi M, Gornbein JA, Calcaterra TC, Slamon DJ, Wang MB, Srivatsan ES. Cyclin D1 amplification and p16(MTS1/CDK4I) deletion correlate with poor prognosis in head and neck tumors.Laryngoscope2002;112:472-81.
15. Weinberger PM, Yu Z, Haffty BG, Kowalski D, Harigopal M, Sasaki C, Rimm DL, Psyrri A. Prognostic significance of p16 protein levels in oropharyngeal squamous cell cancer.Clin Cancer Res2004;10:5684-91.
16. Lassen P, Eriksen JG, Hamilton-Dutoit S, Tramm T, Alsner J, Overgaard J. Effect of HPV-associated p16INK4A expression on response to radiotherapy and survival in squamous cell carcinoma of the head and neck.J Clin Oncol2009;27:1992-8.
17. Kreimer AR, Clifford GM, Boyle P, Franceschi S. Human papillomavirus types in head and neck squamous cell carcinomas worldwide: a systematic review.Cancer Epidemiol Biomarkers Prev2005;14:467-75.
18. Evans JF, Shah JP. Epidermoid carcinoma of the palate.Am J Surg1981;142:451-5.
19. Cady B, Catlin D. Epidermoid carcinoma of the gum. A 20-year survey.Cancer1969;23:551-69.
20. Hiratsuka H, Miyakawa A, Nakamori K, Kido Y, Sunakawa H, Kohama G. Multivariate analysis of occult lymph node metastasis as a prognostic indicator for patients with squamous cell carcinoma of the oral cavity.Cancer1997;80:351-6.
21. Wallwork BD, Anderson SR, Coman WB. Squamous cell carcinoma of the floor of the mouth: tumour thickness and the rate of cervical metastasis.ANZ J Surg2007;77:761-4.
22. Pitman KT. Rationale for elective neck dissection.Am J Otolaryngol2000;21:31-7.
23. Weiss MH, Harrison LB, Isaacs RS. Use of decision analysis in planning a management strategy for the stage N0 neck.Arch Otolaryngol Head Neck Surg1994;120:699-702.
24. Haddadin KJ, Soutar DS, Oliver RJ, Webster MH, Robertson AG, MacDonald DG. Improved survival for patients with clinically T1/T2,N0 tongue tumors undergoing a prophylactic neck dissection.Head Neck1999;21:517-25.
25. Yuen AP, Wei WI, Wong YM, Tang KC. Elective neck dissection versus observation in the treatment of early oral tongue carcinoma.Head Neck1997;19:583-8.
26. Capote A, Escorial V, Munoz-Guerra MF, Rodriguez-Campo FJ, Gamallo C, Naval L. Elective neck dissection in early-stage oral squamous cell carcinoma--does it influence recurrence and survival?Head Neck2007;29:3-11.
27. Janeway HH. The treatment of tumors of the superior maxilla.Ann Surg1918;68:353.
28. Martin H. Cancer of the gums (gingivae).Am J Surg (Special Monograph)1941;54:770-806.
29. Soo KC, Spiro RH, King W, Harvey W, Strong EW. Squamous carcinoma of the gums.Am J Surg1988;156:281-5.
30. Evans JF, Shah JP. Epidermoid carcinoma of the palate.Am J Surg1981;142:451-5.
31. Joe JK, Patel SG, Shaha AR. Management of the neck. In: Rhys Evans PH, Montgomery PQ, Gullane PJ, editors. Principles and Practices of Head and Neck Surgery and Oncology. London and New York: Taylor & Francis; 2003. p. 534-73.
32. Sparano A, Weinstein G, Chalian A, Yodul M, Weber R. Multivariate predictors of occult neck metastasis in early oral tongue cancer.Otolaryngol Head Neck Surg2004;131:472-6.
33. Pentenero M, Gandolfo S, Carrozzo M. Importance of tumor thickness and depth of invasion in nodal involvement and prognosis of oral squamous cell carcinoma: a review of the literature.Head Neck2005;27:1080-91.
34. Andersen PE, Cambronero E, Shaha AR, Shah JP. The extent of neck disease after regional failure during observation of the N0 neck.Am J Surg1996;172:689-91.
35. Jerjes W, Upile T, Petrie A, Riskalla A, Hamdoon Z, Vourvachis M, Karavidas K, Jay A, Sandison A, Thomas GJ, Kalavrezos N, Hopper C. Clinicopathological parameters, recurrence, locoregional and distant metastasis in 115 T1-T2 oral squamous cell carcinoma patients.Head Neck Oncol2010;2:1.
36. Os AD, Karakullukcu B, Leemans CR, Halmos GB, Roodenburg JL, Weert SV, Karagozoglu KH, Witjes MJ. Management of the clinically N0 neck in squamous cell carcinoma of the maxillary alveolus and hard palate.Head Neck2016;38:1794-8.
37. Massano J, Regateiro FS, Januario G, Ferreira A. Oral squamous cell carcinoma: review of prognostic and predictive factors.Oral Surg Oral Med Oral Pathol Oral Radiol Endod2006;102:67-76.
38. Jones HB, Sykes A, Bayman N, Sloan P, Swindell R, Patel M, Musgrove B. The impact of lymphovascular invasion on survival in oral carcinoma.Oral Oncol2009;45:10-5.
39. Sturgis EM, Cinciripini PM. Trends in head and neck cancer incidence in relation to smoking prevalence.Cancer2007;110:1429-35.
40. D’Souza G, Kreimer AR, Viscidi R, Pawlita M, Fakhry C, Koch WM, Westra WH, Gillison ML. Case-control study of human papillomavirus and oropharyngeal cancer.N Engl J Med2007;356:1944-56.
41. Worden FP, Kumar B, Lee JS, Wolf GT, Cordell KG, Taylor JM, Urba SG, Eisbruch A, Teknos TN, Chepeha DB, Prince ME, Tsien CI, D’Silva NJ, Yang K, Kurnit DM, Mason HL, Miller TH, Wallace NE, Bradford CR, Carey TE. Chemoselection as a strategy for organ preservation in advanced oropharynx cancer: response and survival positively associated with HPV16 copy number.J Clin Oncol2008;26:3138-46.
42. Begum S, Gillison ML, Ansari-Lari MA, Shah K, Westra WH. Detection of human papillomavirus in cervical lymph nodes: a highly effective strategy for localizing site of tumor origin.Clin Cancer Res2003;9:6469-75.
43. Rischin D, Young RJ, Fisher R, Fox SB, Le QT, Peters LJ, Solomon B, Choi J, O’Sullivan B, Kenny LM, McArthur GA. Prognostic significance of p16INK4A and human papillomavirus in patients with oropharyngeal cancer treated on TROG 02.02 phase III trial.J Clin Oncol2010;28:4142-8.
44. Lassen P, Overgaard J, Eriksen JG. Expression of EGFR and HPV-associated p16 in oropharyngeal carcinoma: correlation and influence on prognosis after radiotherapy in the randomized DAHANCA 5 and 7 trials.Radiother Oncol2013;108:489-94.
45. Chung CH, Zhang Q, Kong CS, Harris J, Fertig EJ, Harari PM, Wang D, Redmond KP, Shenouda G, Trotti A, Raben D, Gillison ML,Jordan RC, Le QT. p16 protein expression and human papillomavirus status as prognostic biomarkers of nonoropharyngeal head and neck squamous cell carcinoma.J Clin Oncol2014;32:3930-8.
 Journal of Cancer Metastasis and Treatment2018年3期
Journal of Cancer Metastasis and Treatment2018年3期
- Journal of Cancer Metastasis and Treatment的其它文章
- AUTHOR INSTRUCTIONS
- Targeting adenosine receptor 2B in triple negative breast cancer
- The magnitude of benefit from adding taxanes to anthracycIines in the adjuvant settings of breast cancer: discussion of Iarge triaIs and meta-anaIyses
- Pharmacogenomics in colorectal cancer: current role in clinical practice and future perspectives
- Current challenges and opportunities in treating hypoxic prostate tumors
