Postoperative day one serum alanine aminotransferase does not predict patient morbidity and mortality after elective liver resection in non-cirrhotic patients
Ricky Harminder Bhogal, Amit Nair, Davide Papis, Zaed Hamady, Jawad Ahmad, For Tai Lam, Saboor Khan and Gabriele Marangoni
Coventry, UK
Postoperative day one serum alanine aminotransferase does not predict patient morbidity and mortality after elective liver resection in non-cirrhotic patients
Ricky Harminder Bhogal, Amit Nair, Davide Papis, Zaed Hamady, Jawad Ahmad, For Tai Lam, Saboor Khan and Gabriele Marangoni
Coventry, UK
Serum aminotransferases have been used as surrogate markers for liver ischemia-reperfusion injury that follows liver surgery. Some studies have suggested that rises in serum alanine aminotransferase (ALT) correlate with patient outcome after liver resection. We assessed whether postoperative day 1 (POD 1) ALT could be used to predict patient morbidity and mortality following liver resection. We reviewed our prospectively held database and included consecutive adult patients undergoing elective liver resection in our institution between January 2013 and December 2014. Primary outcome assessed was correlation of POD 1 ALT with patient’s morbidity and mortality. We also assessed whether concurrent radiofrequency ablation, neoadjuvant chemotherapy and use of the Pringle maneuver significantly affected the level of POD 1 ALT. A total of 110 liver resections were included in the study. The overall in-hospital patient morbidity and mortality were 31.8% and 0.9%, respectively. The median level of POD 1 ALT was 275 IU/L. No correlation was found between POD 1 serum ALT levels and patient morbidity after elective liver resection, whilst correlation with mortality was not possible because of the low number of mortalities. Patients undergoing concurrent radiofrequency ablation were noted to have an increased level of POD 1 serum ALT but not those given neoadjuvant chemotherapy and those in whom the Pringle maneuver was used. Our study demonstrates POD 1 serum ALT does not correlate with patient morbidity after elective liver resection.
alanine aminotransferase;
hepatectomy;
reperfusion injury;
aminotransferases;
postoperative complications
Introduction
Liver resection is the only potential cure in patients with liver-only-metastatic colorectal liver disease.[1]Despite improvements in anesthetic and surgical techniques the mortality and morbidity in patients following liver resection still ranges from 0% to 8% and 14% to 47%, respectively.[2-4]Early prediction and management of postoperative complications are crucial for the improvement of short-term patient outcome[5]and prediction and treatment of early morbidity improve the long-term outcome in patients who undergo liver resection.[6]There are several scoring systems and predictive models aimed at predicting complications and patient morbidity after elective liver resection.[7]Some of these scoring systems include assessing peak postoperative serum bilirubin,[8]the so called “50-50 criteria” (serum bilirubin concentration >50 μmol/L and prothrombin time <50%)[9]and the International Study Group of Liver Surgery score.[10]A recent study[11]demonstrated
that serum biomarkers such as Ki67 and KRAS can correlate with patient outcome after liver resection. These scoring systems are dependent on the measurement of multiple hematological and biochemical parameters several days after surgery, which limit their use in routine clinical practice. Postoperative serum aminotransferases level after liver resections would be an attractive marker in view of its simplicity of use. Reissfelder et al[12]suggested that although serum aminotransferases (e.g., ALT and AST) usually return to basal values during the first postoperative days 5 to 7 after liver resection, significant differences in their levels may be observed as early as postoperative day 1 (POD 1) between patients and could be used to predict postoperative complications. The aim of the present study was therefore to evaluate the prognostic significance of the serum ALT level on POD 1 for patient morbidity and mortality after elective liver resection in a cohort of patients.

Table 1. Characteristics of the 110 patients who underwent elective liver resection (n, %)
Methods
We reviewed our prospectively maintained database and included all patients undergoing elective liver resection at our institution between January 1, 2013 and December 31, 2014. There were 114 adult patients who underwent liver resection within the study period. Of these, 4 patients underwent synchronous pancreas and liver surgery and were excluded from the final analysis. At last, 110 patients were investigated.
The primary endpoint of the study was POD 1 serum ALT level. The secondary endpoint was in-hospital postoperative outcome according to the Clavien-Dindo classification.[13]Demographics, selected preoperative parameters and selected intraoperative parameters of the patients are shown in Table 1.
Continuous variables were expressed as a median with interquartile range (IQR). Discrete variables were expressed as counts (n) and percentages (%). Dependent variables were the study endpoints. Clavien-Dindo morbidity grade was treated as a categorical variable. POD 1 serum ALT levels were treated as a continuous variable. Statistical analysis was performed using IBM SPSS Statistics for Windows version 22.0 (Armonk, NY: IBM Corp).
Results
Characteristics of the 110 patients analyzed are summarized in Table 1. Indication for liver resection was malignancy in 96 (87.3%) patients and the resection was a major hepatectomy in 29 (26.4%) patients. Preoperative chemotherapy was given to 55 (50.0%) patients. Eleven (10.0%) patients had undergone a previous liver resection. Nine (8.2%) patients had a laparoscopic liver resection. Intermittent portal triad clamping was performed in 55 (50.0%) patients. When used, inflow occlusion lasted a median of 18 minutes (IQR: 10-25). The median blood loss was 300 mL (IQR: 150-487), and 8 patients (7.3%) required blood transfusions. Seventeen (15.5%) liver resections were performed with concomitant radiofrequency ablation. The overall morbidity was 31.8% (n=35) and mortality 0.9% (n=1). Thirty-five patients
suffered from postoperative morbidity. The in-patient death in our series was a 68-year-old male patient who underwent a right hemi-hepatectomy and Roux-en-Y reconstruction for a hilar cholangiocarcinoma. The patient died from systemic sepsis and multi-organ failure 18 days after surgery (Table 2).
The median POD 1 serum ALT level was 275 IU/L (IQR: 159-510). The POD 1 ALT level was not significantly different between the patients who developed complications and those who did not (Table 3). We subsequently assessed whether POD 1 serum ALT varied in patients who had received neoadjuvant chemotherapy, concurrent intraoperative radiofrequency ablation, or the Pringle maneuver during elective liver resection. The POD 1 serum ALT level was significantly higher in patients who underwent intraoperative radiofrequency ablation (P<0.0001), but no difference was found between the patients who received neoadjuvant chemotherapy and those who were subjected to the Pringle maneuver (Figs. 1-3). Blood loss (P<0.01), operative time (P<0.01) and BMI (P<0.05) were also associated with an increase in POD 1 serum ALT level although Spearman’s rho was as weak as 0.406, 0.504 and 0.313, respectively. Intraoperative blood transfusion was also associated with higher serum POD 1 serum ALT level (P<0.05). The POD 1 serum ALT level was associated with an increased POD 1 serum bilirubin level although Spearman’s rho was as weak as 0.356. POD 1 serum ALT level was not associated with POD 5 serum bilirubin level (P=0.16 and Spearman’ s rho 0.248). Finally, POD 1 serum ALT level was not associated with the extent of liver resection.

Fig. 1. POD 1 serum ALT in patients in whom concurrent radiofrequency ablation was used. POD 1 serum ALT levels in patients who had (right, n=17) and those who had not (left, n=93) received concurrent radiofrequency ablation (P<0.0001).
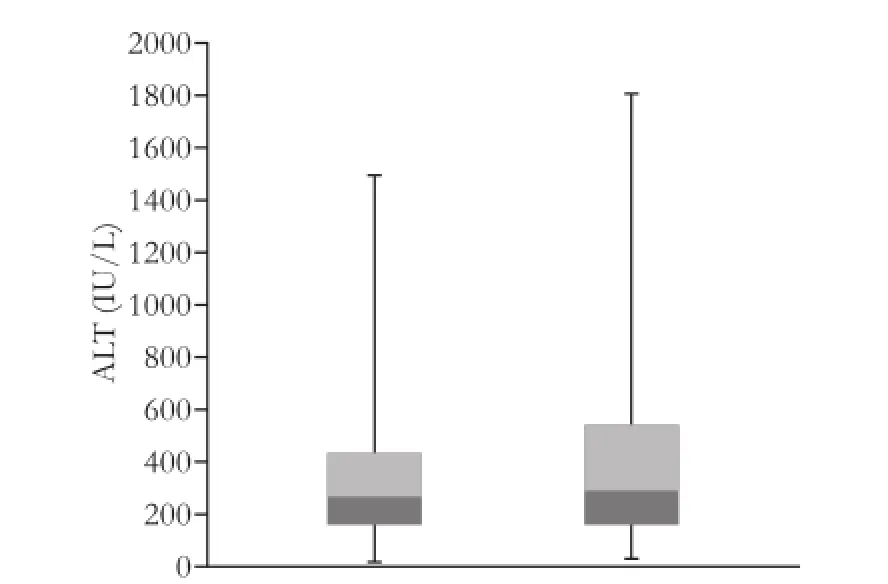
Fig. 2. POD 1 serum ALT levels in patients who were subjected to neoadjuvant chemotherapy. POD 1 serum ALT levels in patients who had (right, n=42) and those who had not (left, n=58) received preoperative neoadjuvant chemotherapy.
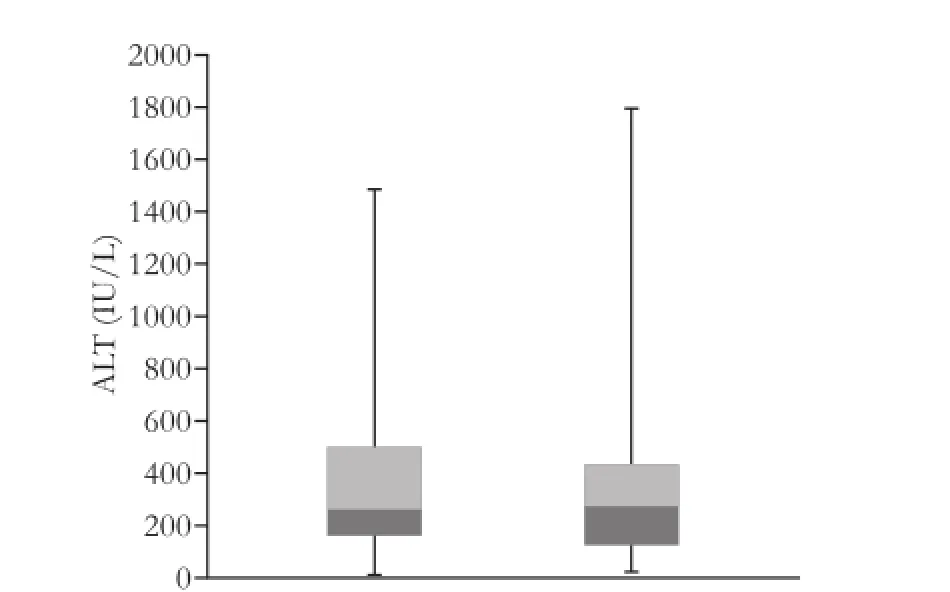
Fig. 3. POD 1 serum ALT in patients in whom the Pringle maneuver was used. POD 1 serum ALT levels in patients who had (right, n=55) and those who had not (left, n=55) used the Pringle maneuver during liver resection.

Table 2. The number and type of complications after elective liver resection
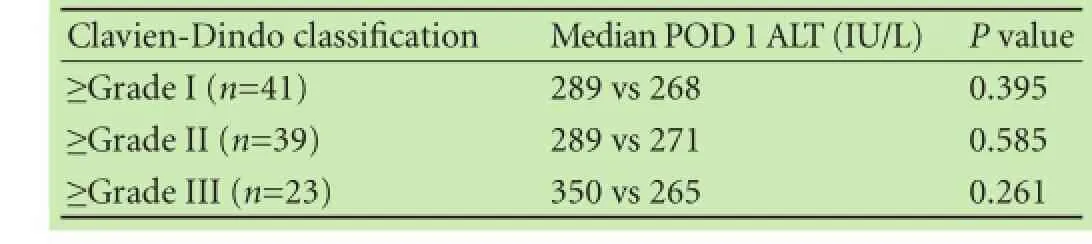
Table 3. POD 1 serum ALT levels in patients with or without complications after liver resection
Discussion
The ability to be able to stratify patients into those at low- and high-risk of complications and/or mortality after elective liver resection would allow individualized, patient centric postoperative management. Serum ALT level has been suggested to reflect liver cytolysis and may provide a surrogate marker for liver injury and hence may correlate with postoperative complications. POD 1 serum ALT level is therefore an attractive marker of morbidity and mortality in view of its simplicity of use.
Previous studies[14,15]have attempted to use model for end-stage liver disease (MELD), ASA classification, Charlson index of co-morbidity, quantitative tests such as idocyanine green and Child-Pugh score to predict morbidity after liver resection with little success. Furthermore, solitary biochemical markers such as C-reactive protein have been used to assess long-term patient outcome rather than postoperative complications.[16]Serum bilirubin and international normalised ratio (INR) have been used to assess the risk of liver failure post-hepatectomy but do not predict postoperative morbidity or mortality.[4]Whether POD 1 serum aminotransferases after hepatectomy can predict short-term patient outcome in routine clinical practice has not been assessed so far.[8,10]Reissfelder et al[12]analyzed 835 consecutive patients who underwent liver resection and found that serum bilirubin and INR, but not ALT, predicted hepatic insufficiency after hepatectomy and some postoperative complications. A further study[6]evaluated the use of postoperative peak aminotransferase to assess whether it was predictive for postoperative complications. The authors concluded after assessing over 650 patients who had undergone liver resections that the peak level of postoperative serum aminotransferases does not correlate with either the use of inflow occlusion or postoperative patient outcome. Importantly, these studies assessed the correlation between peak postoperative serum ALT levels and patient outcome but not POD 1 serum ALT levels like the present study. It is important to state that peak the levels of ALT and POD 1 serum ALT represent different temporal parameters with regard to aminotransferases levels after liver resection.
In our study, POD 1 serum ALT did correlate with the duration of surgery, intraoperative blood loss and concurrent intraoperative ablation, but not neoadjuvant chemotherapy.[17]In addition, we found a significant association of POD 1 serum ALT with intraoperative blood transfusion and high BMI. However, POD 1 serum ALT was not correlated with patient morbidity or mortality after elective liver resection. There was a limited use of postoperative ALT in stratifying patient risk after liver resection although this may be due to the relatively low frequency of blood transfusion in our series (7.3%). Unfortunately because of the relative low number of patients in our series, we were not able to conduct multiregression analysis to assess the effects of the above factors on POD 1 serum ALT. There is an urgent need for immediate measurable biomarkers that can accurately predict morbidity after liver surgery.[11]There are several reports[18,19]on novel biomarkers in pre-clinical settings that may in the future be used to assess liver ischemia during resection such as argininosuccinate synthase and microRNA-122. However, it is difficult to predict whether these novel biomarkers will be effective and easy to measure in the clinical setting.
There are inherent limitations in our study, a single center retrospective study. Further work is required to develop a user-friendly scoring system that will accurately predict patient outcome after liver resection. Patients undergoing liver resection are also a heterogeneous group, and devising a single prognostic scoring system may not be feasible. In our series there was one death, and hence multiple logistic regression analyses could not be used to evaluate the use of POD 1 serum ALT in predicting mortality.
In conclusion, POD 1 serum ALT does not seem to allow stratification of patients into low- and high-risk groups of morbidity after elective liver resection.
Contributors: HZ, LFT, KS and MG proposed the study. BRH, NA, PD and MG performed research and wrote the first draft. NA, AJ, LFT, KS and MG collected and analyzed the data. All authors contributed to the design and interpretation of the study and to further drafts. MG is the guarantor.
Funding: None.
Ethical approval: This study was approved by the Ethics Committee of the University Hospitals of Coventry and Warwickshire.
Competing interest: No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Khan K, Wale A, Brown G, Chau I. Colorectal cancer with liver metastases: neoadjuvant chemotherapy, surgical resection first or palliation alone? World J Gastroenterol 2014;20:12391-12406.
2 Aloia TA, Fahy BN, Fischer CP, Jones SL, Duchini A, Galati J, et al. Predicting poor outcome following hepatectomy: analysis of 2313 hepatectomies in the NSQIP database. HPB (Oxford) 2009;11:510-515.
3 Breitenstein S, DeOliveira ML, Raptis DA, Slankamenac K, Kambakamba P, Nerl J, et al. Novel and simple preoperative score predicting complications after liver resection in noncirrhotic patients. Ann Surg 2010;252:726-734.
4 Gr?t M, Ho?ówko W, Lewandowski Z, Kornasiewicz O, Barski K, Skalski M, et al. Early post-operative prediction of morbidity and mortality after a major liver resection for colorectal me-
tastases. HPB (Oxford) 2013;15:352-358.
5 de Haas RJ, Wicherts DA, Andreani P, Pascal G, Saliba F, Ichai P, et al. Impact of expanding criteria for resectability of colorectal metastases on short- and long-term outcomes after hepatic resection. Ann Surg 2011;253:1069-1079.
6 Boleslawski E, Vibert E, Pruvot FR, Le Treut YP, Scatton O, Laurent C, et al. Relevance of postoperative peak transaminase after elective hepatectomy. Ann Surg 2014;260:815-821.
7 Yang P, Wu D, Xia Y, Li J, Wang K, Yan Z, et al. A prognostic scoring system for patients with multiple hepatocellular carcinomas treated by hepatectomy. Ann Surg Oncol 2015;22:826-833.
8 Mullen JT, Ribero D, Reddy SK, Donadon M, Zorzi D, Gautam S, et al. Hepatic insufficiency and mortality in 1059 noncirrhotic patients undergoing major hepatectomy. J Am Coll Surg 2007;204:854-864.
9 Balzan S, Belghiti J, Farges O, Ogata S, Sauvanet A, Delefosse D, et al. The “50-50 criteria” on postoperative day 5: an accurate predictor of liver failure and death after hepatectomy. Ann Surg 2005;242:824-829.
10 Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R, et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 2011;149:713-724.
11 Spolverato G, Ejaz A, Azad N, Pawlik TM. Surgery for colorectal liver metastases: the evolution of determining prognosis. World J Gastrointest Oncol 2013;5:207-221.
12 Reissfelder C, Rahbari NN, Koch M, Kofler B, Sutedja N, Elbers H, et al. Postoperative course and clinical significance of biochemical blood tests following hepatic resection. Br J Surg 2011;98:836-844.
13 Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205-213.
14 Schroeder RA, Marroquin CE, Bute BP, Khuri S, Henderson WG, Kuo PC. Predictive indices of morbidity and mortality after liver resection. Ann Surg 2006;243:373-379.
15 Ercolani G, Grazi GL, Callivà R, Pierangeli F, Cescon M, Cavallari A, et al. The lidocaine (MEGX) test as an index of hepatic function: its clinical usefulness in liver surgery. Surgery 2000;127:464-471.
16 Shiba H, Furukawa K, Fujiwara Y, Futagawa Y, Haruki K, Wakiyama S, et al. Postoperative peak serum C-reactive protein predicts outcome of hepatic resection for hepatocellular carcinoma. Anticancer Res 2013;33:705-709.
17 Grat M, Grzegorczyk K, Lewandowski Z, Sujecki D, Szwedowski D, Boltuc A, et al. Intraoperative injuries during liver resection: analysis of 1,005 procedures. Hepatol Int 2011;6:498-504.
18 Prima V, Cao M, Svetlov SI. ASS and SULT2A1 are novel and sensitive biomarkers of acute hepatic injury-a comparative study in animal models. J Liver 2013;2:1000115.
19 Van Caster P, Brandenburger T, Strahl T, Metzger S, Bauer I, Pannen B, et al. Circulating microRNA-122, -21 and -223 as potential markers of liver injury following warm ischaemia and reperfusion in rats. Mol Med Rep 2015;12:3146-3150.
Received July 17, 2015
Accepted after revision February 2, 2016
(Hepatobiliary Pancreat Dis Int 2016;15:655-659)
Author Affiliations: Department of Hepato-pancreatico-biliary Surgery, University Hospitals of Coventry and Warwickshire, Clifford Bridge Road, Coventry, West Midlands, CV2 2DX, UK (Bhogal RH, Nair A, Papis D, Hamady Z, Ahmad J, Lam FT, Khan S and Marangoni G); and University of Birmingham, Centre for Liver Research, Institute for Biomedical Research, The Medical School, Edgbaston, Birmingham, West Midlands, B15 2TT, UK (Bhogal RH)
Gabriele Marangoni, MD, Department of Hepatopancreatico-biliary Surgery, University Hospitals Coventry and Warwickshire, Clifford Bridge Road, Coventry, West Midlands, CV2 2DX, UK (Tel: +44-2476965269; Fax: +44-2476965150; Email: Gabriele.Marangoni@uhcw. nhs.uk)
? 2016, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(16)60090-5
Published online May 9, 2016.
 Hepatobiliary & Pancreatic Diseases International2016年6期
Hepatobiliary & Pancreatic Diseases International2016年6期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- Hepatic perivascular epithelioid cell tumor in three patients
- Uncoupling protein 2 deficiency reduces proliferative capacity of murine pancreatic stellate cells
- Jagged1 and DLL4 expressions in benign and malignant pancreatic lesions and their clinicopathological significance
- Endoscopic bilateral stent-in-stent placement for malignant hilar obstruction using a large cell type stent
- Prognosis of hepatocellular carcinoma with bile duct tumor thrombus after R0 resection: a matched study
- Urgent ERCP for acute cholangitis reduces mortality and hospital stay in elderly and very elderly patients
