Clinicopathologic and molecular characteristics of 44 patients with pure secretory breast carcinoma
Lijuan Li, Nan Wu, Fangxuan Li, Lingmei Li, Lijuan Wei, Juntian Liu
1Department of Cancer Prevention Center; 2Department of Pathology, Tianjin Medical University Cancer Institute and Hospital, National Clinical Research Center for Cancer, Key Laboratory of Cancer Prevention and Therapy, Tianjin, Tianjin's Clinical Research Center for Cancer, Key Laboratory of Breast Cancer Prevention and Therapy, Tianjin Medical University,Ministry of Education, Tianjin 300060, China
ABSTRACT Objective:Secretory breast carcinoma (SBC) is a rare type of breast malignancy, accounting for less than 0.02% of all infiltrating breast malignancies. The pure SBC, a type of SBC without another type of breast malignant neoplasm, is particularly rare. This study aimed to investigate the clinicopathologic and molecular features of pure SBC.Methods:The main pathological parameters such as estrogen receptor (ER), progesterone receptor (PR), and human epithelial growth factor receptor 2 (C-erbB-2) were detected by immunohistochemistry (IHC), and the clinicopathologic and prognostic difference were compared with invasive ductal carcinoma (IDC). Fluorescent in situ hybridization (FISH) and reverse transcription polymerase chain reaction (RT-PCR) was performed to identify the ETV6-NTRK3 rearrangement of SBC.Results:We found that the positivity rates of ER, PR, C-erbB-2, p53, and S-100 were 47.7% (21/44), 52.3% (23/44), 36.4%(16/44), 27.3% (12/44), and 95.5% (42/44), respectively, which were higher than those reported in previous studies. Special periodic acid-Schiff analysis was performed in 36 patients, and the value of the Ki-67 index ranged from 1% to 50% (mean value:10%). Interestingly, most patients with pure SBC harbored an ETV6-NTRK3 rearrangement with an 88.6% (39/44) expression rate. Compared with IDC, the tumor size of most patients with SBC was larger than 2 cm (P = 0.024). Ultrasound showed benign lesions, and the total misdiagnosis rate was higher (P = 0.020). Although the pathological classification was mostly triple-negative breast cancers (P = 0.036), there was less metastasis (P = 0.029), and the overall prognosis was better than that of the IDC group.Conclusions:Although axillary lymph node metastasis, local recurrence, or distant metastasis may occur, SBC is also considered an indolent neoplasm with a good prognosis. Once diagnosed, surgical treatment should be performed as soon as possible,followed by appropriate adjuvant chemotherapy, irradiation, and endocrine therapies.
KEYWORDS Breast cancer; pure secretory breast carcinoma; clinicopathologic feature; therapeutics and prognosis
Introduction
Secretory breast carcinoma (SBC) is a rare and distinct variant of breast cancer, accounting for less than 0.02% of all breast cancers1. It was first reported as “juvenile breast carcinoma” by McDivitt in 19662. However, it was later shown to occur in all age groups, and both men and women can be affected. Consequently, the term “juvenile breast cancer” was replaced by the term “secretory breast cancer.”The 2012 World Health Organization (WHO) Classification of Tumors of the Breast adopted the terminology and defined SBC as a rare, low-grade, translocation-associated invasive carcinoma, classified as epithelial tumors, and the ICD-O code was 8502/3. It is characterized by a large amount of eosinophilic secretory material inside or outside the cancer cells, which stains positively with periodic acid-Schiff (PAS)and diastase-PAS (D-PAS) or Alcian blue (AB). SBC has been reported to display an immunophenotype with triple negativity. Unlike the other triple-negative breast cancers(TNBCs), the prognosis of SBC is better3. In addition, the morbidity of pure SBC (PSBC) is lower. PSBC is considered a type of SBC without other pathological types. Because the diagnosis of this disease is comparatively limited, it is difficult to separate from other pathological types. To date, due to the rarity of SBC and PSBC in particular, there have been only a few cases reported or separate analyses in the literature. Here, we reviewed our archived breast cancer materials and identified 44 such cases. This study aimed to describe the clinicopathologic and molecular features and investigate the role of comprehensive therapy in the management of this disease.
Materials and methods
Clinicopathological data
A total of 28,364 cases of breast cancer were diagnosed from January 1986 to October 2014 at the Department of Breast Cancer, Tianjin Medical University Cancer Institute and Hospital (Tianjin, China). Forty-four cases were diagnosed as SBC, according to the 2012 WHO Classification of Tumors of the Breast. The histopathology of the tumors was reviewed independently by at least two pathologists. The majority of patients were women except for three male patients (the age of the three men was 11, 61, and 69 years), and the median age was 48 years (range: 4-76 years). A total of 88 patients with invasive ductal carcinoma (IDC) were randomly selected as the control group. The female patients' ages during the initial examination ranged from 6 to 78 years(median: 48 years). None of the patients received radiotherapy, chemotherapy, or endocrine therapy before surgery. Available data including clinical presentations,therapeutic regimens, and follow-up information were evaluated from the date of initial diagnosis until the patient's death or the most recent censorship. This study was approved by the Ethics Committee of Tianjin Medical University Cancer Institute and Hospital. Written consents were obtained from each patient.
Imaging and histopathological study
Most of the patients were examined by mammography and/or ultrasound before surgery, except for three who underwent mastectomy or lumpectomy before hospitalization. All tissues were removed and fixed in 10%formalin, embedded in paraffin, sectioned at a thickness of 5 μ m or 10 μ m, and stained with hematoxylin and eosin.Immunohistochemistry (IHC) was performed to analyze estrogen receptor (ER), progesterone receptor (PR), human epithelial growth factor receptor 2 (C-erbB-2) Ki-67, and p53(Zymed, San Francisco, CA, USA) in all patients, while S-100(Zymed, San Francisco, CA) and special stains for PAS and D-PAS were performed only in SBC patients. The threshold of positivity for ER and PR was 1% for invasive tumor cells4.The American Society of Clinical Oncology/College of American Pathologists (ASCO-CAP) guidelines for the interpretation of C-erbB-2 immunostaining were followed5.The IHC stain was scored as positive if >15% of the tumor cells demonstrated an expression. The positive reaction of S-100 antibodies was classified into one of four grades (0, 1+,2+, and 3+) based on the presence of brown granular staining intensity precipitates within the cytoplasm as well as the percentage of tumor cells that showed a positive reaction.Expression was scored as (-) if no cancer cells were detected or if approximately 0%-10% of tumor cells showed a positive reaction; (1+) if staining showed weak intensity in 11%-50%of tumor cells or moderate intensity in 11%-25% of tumor cells; (2+) if staining showed weak intensity in more than 51% of tumor cells, moderate intensity in 26%-50% of tumor cells, or strong intensity in 11%-25% of tumor cells;and (3+) if staining showed moderate intensity in more than 51% or strong intensity in more than 26% of tumor cells. For the statistical analyses, (-) and (1+) were considered to be a negative stain and (2+) and (3+) to be a positive stain.
Fluorescence in situ hybridization (FISH)
To identify the ETV6-NTRK3 rearrangement of SBC, FISH assay was performed using the Histology FISH Accessory Kit(Dako, Glostrup, Denmark). Briefly, each 5 μm section was deparaffinized in xylene and rehydrated in a 100%, 90%, and 70% ethanol, successively. After washing in phosphatebuffered saline and proteolytic treatment, the tissue section and probes (Abbott, Chicago, IL) were co-denaturated at 85°C for 5 min and then hybridized at 37°C overnight.Probes were visualized as green and red. The next day, nuclei were counterstained with DAPI/antifade solution. Slides were viewed with a DAPI/rhodamine/fluorescein filter, and pictures were captured using a CDD camera, filtered, and processed with Applied Imaging system using an Olympus Microsystems microscope. At least 50 interphase nuclei were analyzed per hybridization.
RNA isolation
Total RNA was extracted from cancer tissues and adjacent normal tissues using the RNeasy? Mini Kit (QIAGEN,Valencia, CA, USA) following the manufacturer's protocol.The integrity of the RNA was determined by electrophoresis.The concentration and purity of the RNA were analyzed by spectrophotometry (NanoDrop 8000, Thermo Scientific,MA, USA). RNA samples were stored at -80°C.
Reverse transcription polymerase chain reaction (RT-PCR)
Total RNA (500 ng) was reverse-transcribed to cDNA using the Takara PrimeScript RT Master Mix Kit (Takara, Tokyo,Japan) following the manufacturer's instruction. About 10 μL samples were performed in a total volume of 50 μL with 10 μL 5× PCR buffer, 28.75 μL sterilized distilled water, 0.25 μL Takara Ex Taq HS, and specific forward and reverse primer 0.5 μL (Table 1), respectively. About 1 cycle of thermal cycling condition was performed within 2 min at 94°C,followed by 50 cycles of 3 PCR steps for 30 seconds at 95°C,30 seconds at 55°C, and 45 seconds at 72°C. Approximately 3% agarose gel was prepared. Then, 5 μL PCR amplification,2 μL buffer, and 1-kbp DNA ladder marker were mixed. The power was switched on, and the voltage was adjusted to 200 V. After 20-30 min, the gel was taken out and photographed.
Statistical analysis
All statistical procedures were conducted using IBM SPSS version 21.0 (Chicago, IL). Survival analysis was performed using the Kaplan-Meier method. Cox regression with covariates survival analysis was performed to determine which parameters yielded an independent predictive value on survival. P-value < 0.05 was considered significant.
Results
Clinical characteristics
The clinicopathologic features of the 44 patients with SBC and 88 with IDC were summarized in Table 2.
Of all the SBC patients, only four were adolescents. The neoplasm was located in the right and left breasts in 23 and 21 patients, respectively. The tumor sizes ranged from 1.5 to 10 cm, with a mean of 3.5 cm. In terms of the TNM staging,28 patients had stages I-IIA, and the remaining 16 had stages IIB-III. Ultrasound examination demonstrated malignant breast lesions in 28 patients, while mammography showed malignant breast lesions in 36 patients. Ultrasound imaging showed round or oval mass with hypoechoic or isoechoic internal echo. Thirty-eight patients underwent modified radical mastectomy or radical mastectomy, and the remaining patients underwent conservative surgery.Lumpectomy was performed in two children (an 11-year-old boy and a 4-year-old girl) and simple mastectomy with axillary lymph node dissection in three patients. Fortypatients underwent postoperative chemotherapy, and eleven had radiotherapy. Of 44 patients, 15 (34.1%) had positive axillary lymph nodes. Compared with IDC, the tumor size of most SBC was larger than 2 cm (P = 0.024). Ultrasound showed benign lesions, and the total misdiagnosis rate was higher (P = 0.020). Although the pathological classification was mostly TNBC (P = 0.036), there was less metastasis (P =0.029), and the overall prognosis was better than that of IDC.

Table 1 Primer sequences used to detect the ETV6-NTRK3 gene fusion by RT-PCR
Histopathological manifestation and molecular features
All patients presented with a painless and firm mass. The cut sections appeared grayish-white to tan or yellow. Axillary lymph node metastasis was detected in 15 patients after thorough axillary dissections; less than three metastatic lymph nodes were observed in eleven patients and more than three in four patients. Histologically, all patients showed characteristic features, and abundant secretory material inside or outside the cancer cells was observed (Figure 1).The secretions from the intracytoplasmic lumina and extracellular compartment of 36 patients were positive for PAS staining, 42 tumors were positive for S-100, and 12 patients were positive for p53 protein. The value of the Ki-67 index ranged from 1% to 50%, with a mean value of approximately 10%. Interestingly, the positive expression rate of ER and PR was high, which was different from those reported in other studies3. In the present study, positive staining for ER and PR was found in 21 and 23 cases,respectively. In addition, 16 patients expressed C-erbB-2(Figure 2). At the molecular level, the positivity rate of FISH was 68.2% in the epithelial cells of SBC (30/44). Moreover,the results of RT-PCR assay with a special gene fusion were concordant in 39 cases (88.6%) (Figure 3).
Follow-up and prognosis
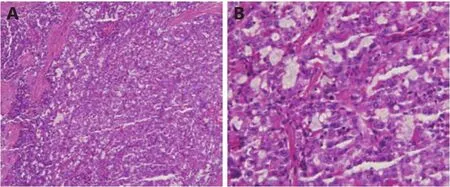
Figure 1 Pure secretory breast carcinoma with intracellular and extracellular secretory material (H&E staining, A, 100 ×; B, 400 ×).
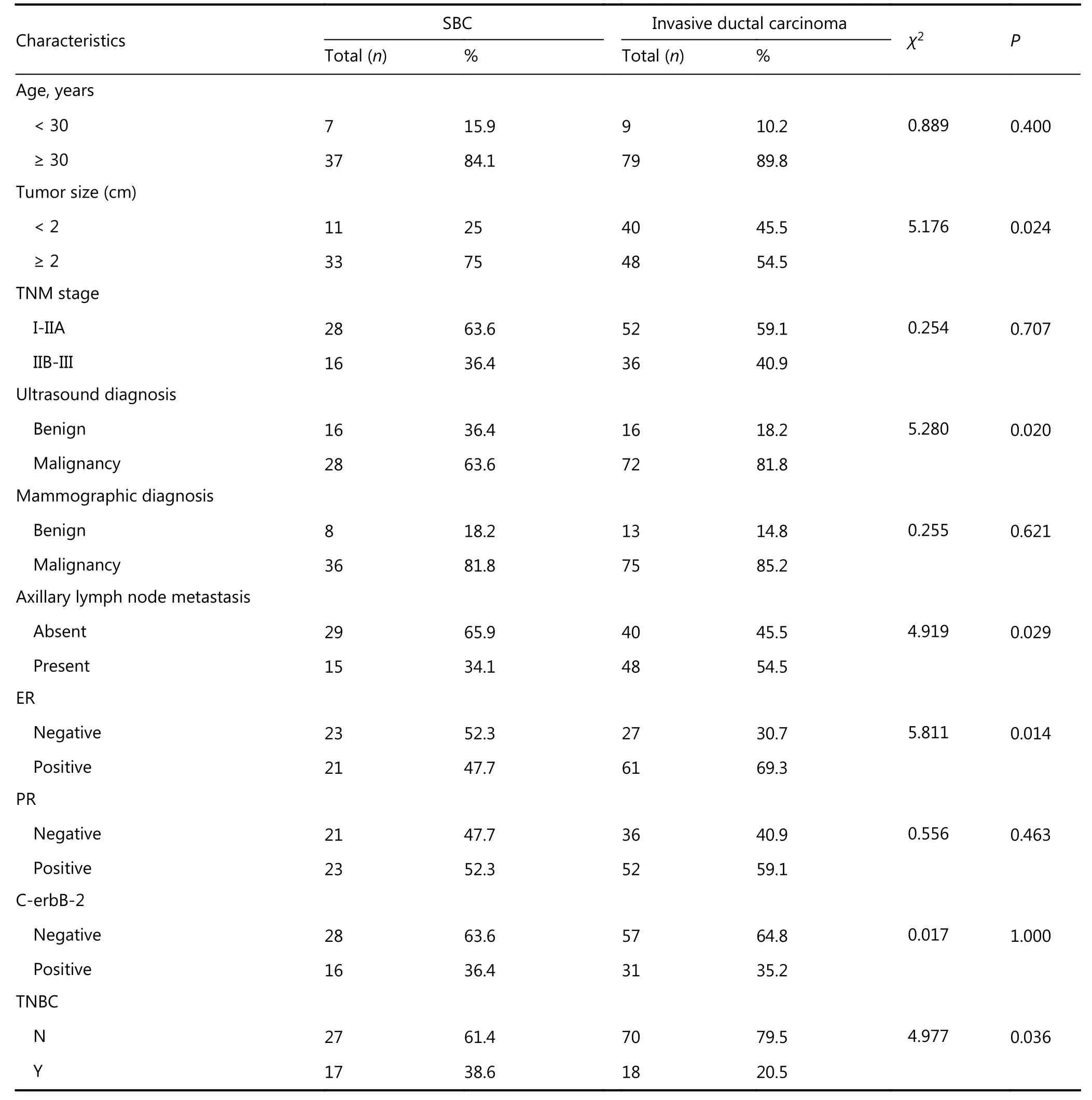
Table 2 Clinicopathological parameters of 44 cases of SBC compared with IDC
Follow-up data were obtained from all patients by hospital visit, telephone interviews, or mail. All data used for calculation were collected from the date of initial diagnosis to the date of death or the most recent censorship. The median follow-up time of SBC patients was 93.4 months (range:10-182 months), whereas that of IDC patients was 94.9 months (range: 12-180 months). Six SBC patients demonstrated evidence of recurrence and distant metastasis;five patients died from cancer and one from Alzheimer's disease. Most of the metastases occurred in the bones (4/6),followed by the liver. Kaplan-Meier analysis showed that the 5-year overall survival (OS) rates of 44 SBC and 88 IDC patients were 93.2% and 87.5%, respectively (P = 0.372). The 10-year OS rates were 88.6% and 75.0%, respectively (P =0.120) (Figure 4). There was no significant difference between the two groups in OS rates, age, tumor size, TNM stage, axillary lymph node status, distant metastasis, and expression of ER, PR, C-erbB-2, and S-100.
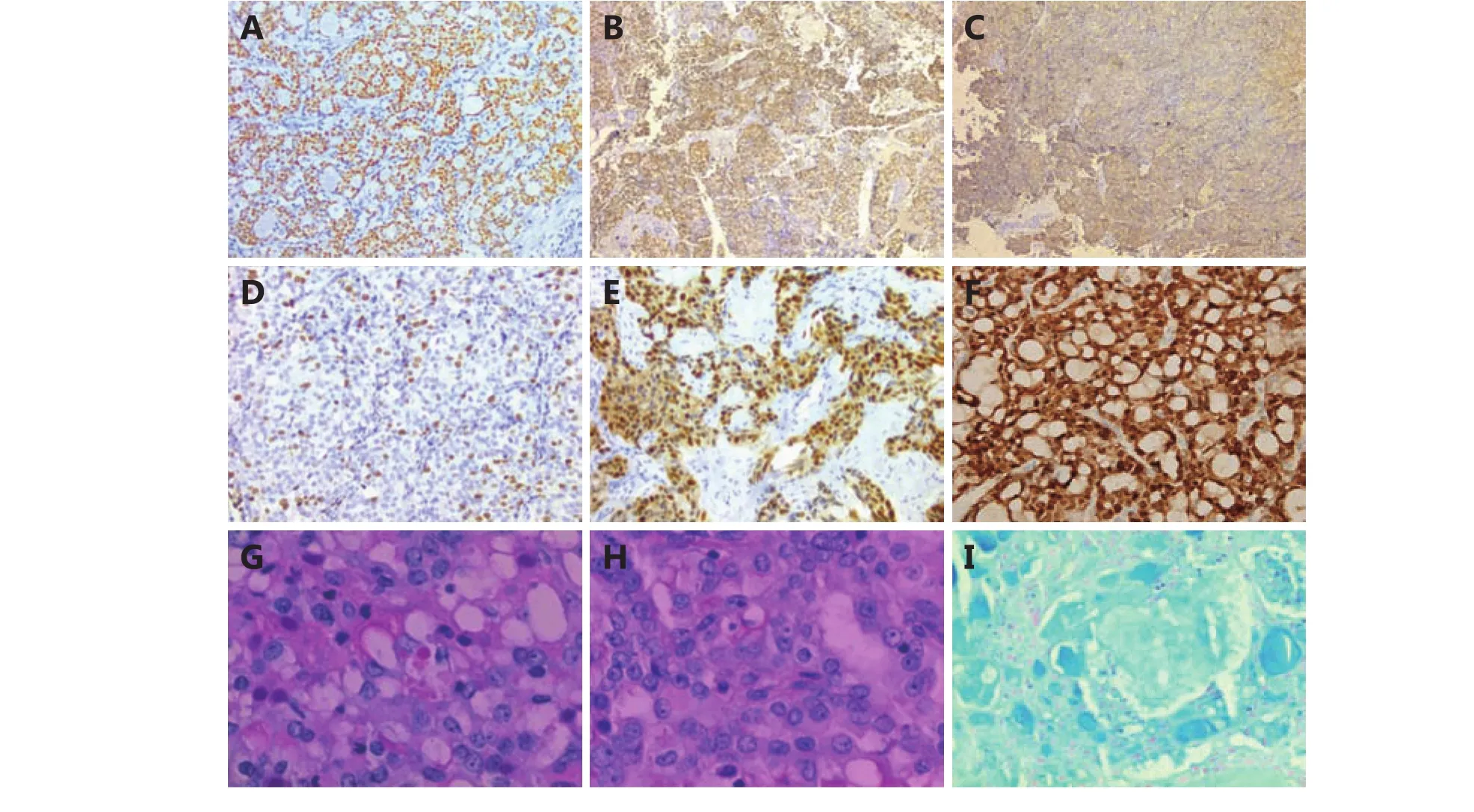
Figure 2 Immunohistochemical features for ER, PR, C-erbB-2, Ki-67, p53, S-100, PAS and D-PAS in the pure secretory breast carcinoma. (A,B) ER and PR is positive on cell nuclei (ER, PR, 100×). (C) C-erbB-2 is positive on cell membrane (3+ staining or 2+ staining with positive FISH) (C-erbB-2, 100 ×). (D, E) Ki-67 and p53 are positive on cell nuclei of PSBC (Ki-67, p53, 400 ×). (F) PSBC with positive immunostaining of S-100 in cell cytoplasm and nuclei (S-100, 400 ×). (G, H, I) A special staining of PAS and D-PAS and Alcian blue are positive in the cytoplasm of PSBC (PAS, D-PAS, AB, 400 ×).
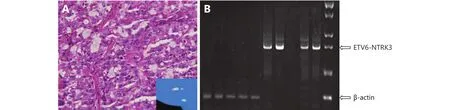
Figure 3 FISH and RT-PCR on paraffin-embedded tumor tissue sections of pure SBC. (A) FISH image showed fusion signal in epithelial cells of SBC, suggesting that it harbored an ETV6-NTRK3 rearrangement. (H&E 400 x, FISH 400 x) (B) RT-PCR: specific ETV6-NTRK3 gene fusion detected.
Discussion
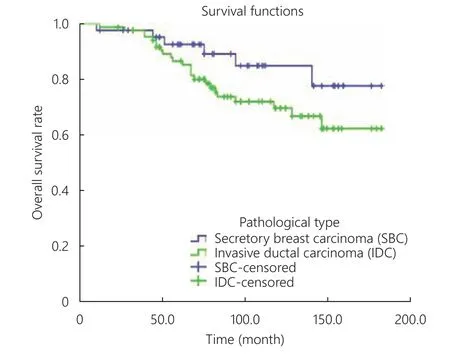
Figure 4 Kaplan-Meier curve of overall survival (OS). There is no significant difference in OS between SBC and IDC (P = 0.131).
Secretory carcinoma is a rare type of breast cancer,accounting for less than 0.02% of all infiltrating breast malignancies, and PSBC is especially rare1,6,7. In our study,the incidence of SBC was 0.15%. To date, very few cases have been reported in the literature. Data accumulation is required to further characterize the tumor and explore how SBC should be treated. In fact, SBC has been reported in a wide range of age groups, between 3 and 86 years old, with a male-to-female ratio of approximately 1 : 68,9, which is higher than the distribution in our data set. Recently, the male-tofemale ratio was demonstrated as 1 : 311. Clinically, these patients presented a painless and firm mass, with a distinct or indistinct circumscription. The rate of tumor growth is relatively slower than other types of breast cancer, and the size ranges from 1 to 16 cm6,10. Previous studies showed that in a large number of individuals, the sonographic feature of SBC is frequently a small, benign-appearing nodule or nodules, and occasionally an intraductal lesion11,12, which may lead to the misdiagnosis of this lesion on sonography. In our retrospective study, we found that of the 27 patients who underwent mammography and ultrasound examination, six were diagnosed with a benign mammary lesion on sonography, and eight with a benign lesion on mammography. The rates of misdiagnosis were 22.2% and 29.6%, respectively. Because of the benign imaging findings,some patients with SBC were not diagnosed. We presumed that this might be related to the distinct circumscription of the tumors. Therefore, imaging examinations to diagnose this disease are comparatively limited. Mammography and ultrasound as individual tests have high rates of misdiagnosis.Therefore, imaging department physicians should combine ultrasound with mammography and increase their vigilance for suspected patients in order to reduce the rate of misdiagnosis in the future.
Currently, the final diagnosis is based on pathological study, which is the “gold standard.” However, considering the specific pathological features of SBC, pathologists should carefully evaluate and differentiate its morphological features from tumors that mimic the histopathologic features of SBC,including lipid-rich carcinoma, acinic cell carcinoma, cystic hypersecretory carcinoma, IDC, glycogen-rich carcinoma,tubular carcinoma, and benign epithelial proliferating lesions, particularly lactational changes or lactating adenoma13,14. The histopathologic feature of this disease is the presence of a large amount of secretory material inside or outside the cancer cells, with positive staining for PAS and DPAS or AB. SBC can show several histological patterns including solid, microcystic, and tubular. Many tumors contain all three patterns with different proportions, and neoplastic cells show minimal atypia and rare mitotic activity15,16. Normally, SBC has been found to be negative for ER and PR, with absence or presence of HER-2 amplification,resembling TNBC. However, it had a strong reaction for S-100 and a low proliferation index, lacking increased Ki-67 expression6,16,17. Meanwhile, other studies have reported that SBC could be positive for ER and PR16,18. Actually, in contrast to a majority of studies, we found higher positivity rates of ER and PR. ER positivity was found in 21 tumors and PR positivity in 23 tumors. Furthermore, compared with the group that expressed ER and/or PR, the negative hormone receptor group had no significant differences in survival and prognosis. Although the pathological classification showed mostly TNBC (P = 0.036), there was less metastasis in SBC(P = 0.029), and the overall prognosis was better than that of IDC. This might be due to the special pathological features of SBC or the limited number of samples, which could cause some deviation from other results. The value of the Ki-67 index ranged from 1% to 50%, with a mean value of approximately 10%. This value was similar to that reported in other studies. Several studies have found an opposite relationship between Ki-67 expression, a biomarker for evaluating cell proliferation in breast cancer, and disease-free survival (DFS) and OS19-21. Those studies suggested that an increase in the expression of Ki-67 in breast cancer cell nuclei increases the risk for recurrence and decreases DFS and OS.Considering this, we suggest that the lack of increased Ki-67 expression may have been associated with inhibition of tumor cell growth and metastasis through different modes of action, thereby leading to a good prognosis in SBC.Remarkably, the typical genomic profile of SBC, an epithelial tumor of the breast, involves the balanced translocation,t(12;15), which creates an ETV6-NTRK3 fusion encoding chimeric tyrosine kinase. This is also encountered in cellular mesoblastic nephroma and infantile fibrosarcoma, which are important for breast cell proliferation and survival. This finding suggests that this kind of SBC is a part of the basallike spectrum22-25. Previous study showed that over 90% of SBC demonstrated this balanced translocation at molecular level24. We enrolled 44 paraffin specimens of SBC by FISH and RT-PCR to detect the balance translocation of ETV6-NTRK3. Interestingly in our study, ETV6 alterations were present in 39 (88.6%) patients with SBC, highlighting their genetic specificity (Figure 3). In addition, the high expression of the ETV6-NTRK3 fusion gene in pure SBC in Asian women suggests that it may be a potential biomarker for differential diagnosis. In the future, FISH could be useful to rule out differential diagnoses such as apocrine carcinoma,lipid- or glycogen-rich lobular, and ductal or mucinous carcinoma and to identify SBC among basal-like carcinomas.
Since the rate of tumor growth is low and the prognosis is good, there is no consensus regarding the treatment of SBC.Surgery is considered the primary treatment for this pathology; however, there are no published guidelines for the extent of surgical management. Furthermore, due to the scarcity of reported cases, the significance of neoadjuvant chemotherapy, adjuvant chemotherapy, and postoperative radiotherapy remains unclear. Breast conservative surgery,modified radical mastectomy, and radical mastectomy are the most frequent procedures in adults, whereas simple mastectomy, local excision with sentinel lymph node biopsy,and complete axillary dissection are potentially adequate in children26. These were the surgical methods performed in our study patients. Li et al.6indicated that sentinel lymph node biopsy was able to evaluate the lymph node status of SBC effectively. The same result was reported in several studies.Tumor size can be used to evaluate axillary lymph node metastasis. If the tumor is less than 2 cm, axillary metastasis is uncommon27.
Soyer et al.28suggested that patients with primary tumors larger than 2 cm should undergo chemotherapy or radiotherapy after surgery. Based on this finding and the biological characteristics of the case, we suggest that conservative surgery with sentinel lymph node biopsy is preferred for tumors less than 2 cm and a mass with wellcircumscribed margins and no suspicion of axillary lymph node metastasis. To some extent, this approach can minimize complications caused by axillary dissection. However, a previous study reported that a young woman experienced local recurrence after undergoing conservative surgery29.Therefore, the status of axillary lymph node must be carefully assessed.
Prior studies found that the 5-year cause specific survival(CSS) was 94.4% and 10-year CSS was 91.4%8. Although as an indolent neoplasm, SBC is less aggressive and has a good outcome, axillary lymph node metastasis, local recurrence,and distant metastasis can occur. Many previous studies described that the incidence rate of axillary lymph node metastasis of SBC was approximately 15%-30%, and most cases involved less than four lymph nodes6,30. Studies have shown that SBC behavior seems to be less aggressive in children than in adults, and lymph node metastasis rarely occurs in adolescents9. Actually, distant metastases from SBC are extremely rare; however, several studies reported chest recurrence or distant metastases appearing as late as 20 years after conventional surgery12,17. Therefore, long-term followup of at least 20 years is recommended10,16. In our study, five patients were still alive with local recurrence or metastasis at the time of analysis. Bone metastasis occurred in three patients and contralateral supraclavicular lymph node metastasis occurred in two patients. These patients underwent a second surgery and were administered pamidronate disodium, respectively. Therefore, after metastasis occurs, timely and effective therapy can still achieve the goal of extending life and improving the quality of life31. Similarly, local recurrence after a long disease-free interval has been described in numerous cases29,32, which is in accordance with our research.
In conclusion, SBC is an uncommon histologic subtype of infiltrating breast malignancy with a specific ETV6-NTRK3 fusion, which has a slow growth pattern and a good prognosis. Due to its rarity, there are no specific imaging and clinical characteristics for this entity. Hence, clinicians should combine the clinical features with imaging examinations to reduce the misdiagnosis rate. Considering the possibility of axillary lymph node metastasis, local recurrence, or distant metastasis, long-term follow-up is advised for SBC in particular. Once diagnosed, surgical treatment should be implemented as soon as possible, and adjuvant chemotherapy, irradiation, and endocrine therapies should be followed appropriately.
Conflict of interest statement
No potential conflicts of interest are disclosed.
 Cancer Biology & Medicine2019年1期
Cancer Biology & Medicine2019年1期
- Cancer Biology & Medicine的其它文章
- Application of next-generation sequencing technology to precision medicine in cancer: joint consensus of the Tumor Biomarker Committee of the Chinese Society of Clinical Oncology
- Methods of computed tomography screening and management of lung cancer in Tianjin: design of a population-based cohort study
- Reactive capillary hemangiomas: a novel dermatologic toxicity following anti-PD-1 treatment with SHR-1210
- Perioperative rh-endostatin with chemotherapy improves the survival of conventional osteosarcoma patients: a prospective non-randomized controlled study
- 68Gallium-labelled PSMA-PET/CT as a diagnostic and clinical decision-making tool in Asian prostate cancer patients following prostatectomy
- Identification of portal vein tumor thrombus with an independent clonal origin in hepatocellular carcinoma via multi-omics data analysis
